Orthostatic hypotension, also known as postural hypotension, is a medical condition wherein a person's blood pressure drops when standing up or sitting down. Primary orthostatic hypotension is also often referred to as neurogenic orthostatic hypotension. The drop in blood pressure may be sudden, within 3 minutes or gradual. It is defined as a fall in systolic blood pressure of at least 20 mmHg or diastolic blood pressure of at least 10 mmHg after 3 minutes of standing. It occurs predominantly by delayed constriction of the lower body blood vessels, which is normally required to maintain adequate blood pressure when changing the position to standing. As a result, blood pools in the blood vessels of the legs for a longer period, and less is returned to the heart, thereby leading to a reduced cardiac output and inadequate blood flow to the brain.

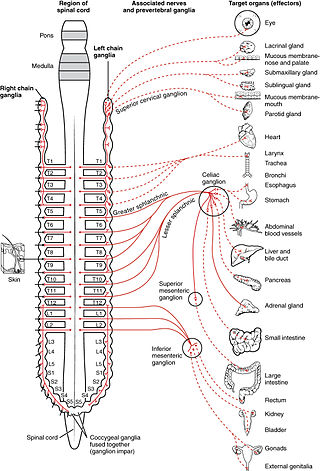
The autonomic nervous system (ANS), sometimes called the visceral nervous system and formerly the vegetative nervous system, is a division of the nervous system that operates internal organs, smooth muscle and glands. The autonomic nervous system is a control system that acts largely unconsciously and regulates bodily functions, such as the heart rate, its force of contraction, digestion, respiratory rate, pupillary response, urination, and sexual arousal. This system is the primary mechanism in control of the fight-or-flight response.

The parasympathetic nervous system (PSNS) is one of the three divisions of the autonomic nervous system, the others being the sympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.
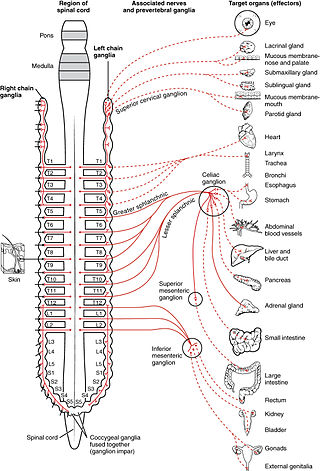
The sympathetic nervous system (SNS) is one of the three divisions of the autonomic nervous system, the others being the parasympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.
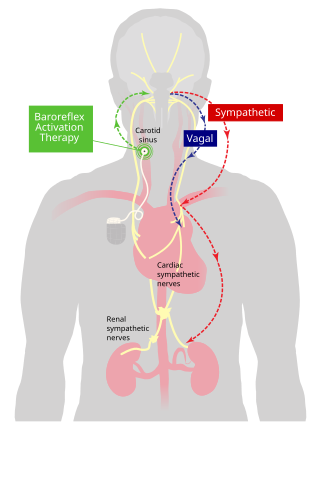
Baroreceptors are sensors located in the carotid sinus and in the aortic arch. They sense the blood pressure and relay the information to the brain, so that a proper blood pressure can be maintained.

The renin–angiotensin system (RAS), or renin–angiotensin–aldosterone system (RAAS), is a hormone system that regulates blood pressure, fluid and electrolyte balance, and systemic vascular resistance.

Heart rate is the frequency of the heartbeat measured by the number of contractions of the heart per minute. The heart rate varies according to the body's physical needs, including the need to absorb oxygen and excrete carbon dioxide. It is also modulated by numerous factors, including genetics, physical fitness, stress or psychological status, diet, drugs, hormonal status, environment, and disease/illness, as well as the interaction between these factors. It is usually equal or close to the pulse rate measured at any peripheral point.
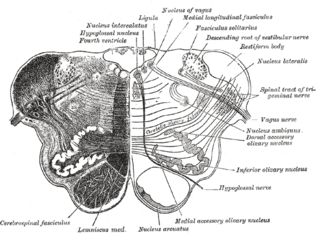
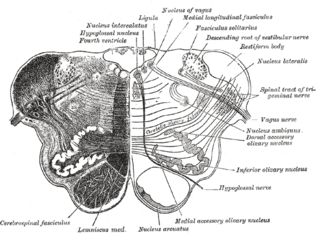
The nucleus ambiguus is a group of large motor neurons, situated deep in the medullary reticular formation named by Jacob Clarke. The nucleus ambiguus contains the cell bodies of neurons that innervate the muscles of the soft palate, pharynx, and larynx which are associated with speech and swallowing. As well as motor neurons, the nucleus ambiguus contains preganglionic parasympathetic neurons which innervate postganglionic parasympathetic neurons in the heart.
The cardiovascular centre is a part of the human brain which regulates heart rate through the nervous and endocrine systems. It is considered one of the vital centres of the medulla oblongata.
Cushing reflex is a physiological nervous system response to increased intracranial pressure (ICP) that results in Cushing's triad of increased blood pressure, irregular breathing, and bradycardia. It is usually seen in the terminal stages of acute head injury and may indicate imminent brain herniation. It can also be seen after the intravenous administration of epinephrine and similar drugs. It was first described in detail by American neurosurgeon Harvey Cushing in 1901.

In human anatomy, the carotid sinus is a dilated area at the base of the internal carotid artery just superior to the bifurcation of the internal carotid and external carotid at the level of the superior border of thyroid cartilage. The carotid sinus extends from the bifurcation to the "true" internal carotid artery. The carotid sinus is sensitive to pressure changes in the arterial blood at this level. It is the major baroreception site in humans and most mammals.
The Bainbridge reflex or Bainbridge effect is a cardiovascular reflex causing an increase in heart rate in response to increased stretching of the wall of the right atrium due to increased filling of the right atrium with venous blood. It is detected by stretch receptors embedded within the wall of the right atrium, and regulated by a center in the medulla oblongata of the brain.
Reflex bradycardia is a bradycardia in response to the baroreceptor reflex, one of the body's homeostatic mechanisms for preventing abnormal increases in blood pressure. In the presence of high mean arterial pressure, the baroreceptor reflex produces a reflex bradycardia as a method of decreasing blood pressure by decreasing cardiac output.
The Bezold–Jarisch reflex involves a variety of cardiovascular and neurological processes which cause hypopnea, hypotension and bradycardia in response to noxious stimuli detected in the cardiac ventricles. The reflex is named after Albert von Bezold and Adolf Jarisch Junior. The significance of the discovery is that it was the first recognition of a chemical (non-mechanical) reflex.
A vagal maneuver is an action used to stimulate the parasympathetic nervous system by activating the vagus nerve. The vagus nerve is the longest nerve of the autonomic nervous system and helps regulate many critical aspects of human physiology, including heart rate, blood pressure, sweating, and digestion through the release of acetylcholine. Common maneuvers that activate the vagus nerve include the Valsalva maneuver and carotid sinus massage, which can serve diagnostic or therapeutic functions.

Pathophysiology is a study which explains the function of the body as it relates to diseases and conditions. The pathophysiology of hypertension is an area which attempts to explain mechanistically the causes of hypertension, which is a chronic disease characterized by elevation of blood pressure. Hypertension can be classified by cause as either essential or secondary. About 90–95% of hypertension is essential hypertension. Some authorities define essential hypertension as that which has no known explanation, while others define its cause as being due to overconsumption of sodium and underconsumption of potassium. Secondary hypertension indicates that the hypertension is a result of a specific underlying condition with a well-known mechanism, such as chronic kidney disease, narrowing of the aorta or kidney arteries, or endocrine disorders such as excess aldosterone, cortisol, or catecholamines. Persistent hypertension is a major risk factor for hypertensive heart disease, coronary artery disease, stroke, aortic aneurysm, peripheral artery disease, and chronic kidney disease.
Low pressure baroreceptors or low pressure receptors are baroreceptors that relay information derived from blood pressure within the autonomic nervous system. They are stimulated by stretching of the vessel wall. They are located in large systemic veins and in the walls of the atria of the heart, and pulmonary vasculature. Low pressure baroreceptors are also referred to as volume receptors and cardiopulmonary baroreceptors.
Cardiac physiology or heart function is the study of healthy, unimpaired function of the heart: involving blood flow; myocardium structure; the electrical conduction system of the heart; the cardiac cycle and cardiac output and how these interact and depend on one another.
Neurocardiology is the study of the neurophysiological, neurological and neuroanatomical aspects of cardiology, including especially the neurological origins of cardiac disorders. The effects of stress on the heart are studied in terms of the heart's interactions with both the peripheral nervous system and the central nervous system.
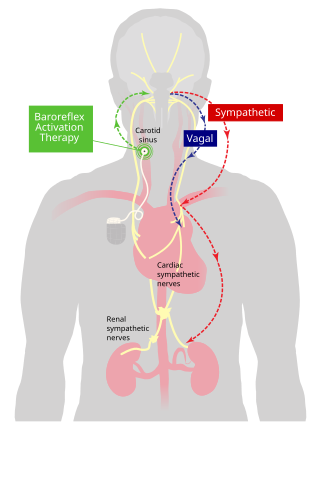
Baroreflex activation therapy is an approach to treating high blood pressure and the symptoms of heart failure. It uses an implanted device to electrically stimulate baroreceptors in the carotid sinus region. This elicits a reflex response through the sympathetic and vagal nervous systems that reduces blood pressure.