Related Research Articles

The peripheral nervous system (PNS) is one of two components that make up the nervous system of bilateral animals, with the other part being the central nervous system (CNS). The PNS consists of the nerves and ganglia outside the brain and spinal cord. The main function of the PNS is to connect the CNS to the limbs and organs, essentially serving as a relay between the brain and spinal cord and the rest of the body. Unlike the CNS, the PNS is not protected by the vertebral column and skull, or by the blood–brain barrier, which leaves it exposed to toxins and mechanical injuries.

The human leg, in the general word sense, is the entire lower limb of the human body, including the foot, thigh and even the hip or gluteal region. However, the definition in human anatomy refers only to the section of the lower limb extending from the knee to the ankle, also known as the crus or, especially in non-technical use, the shank. Legs are used for standing, and all forms of locomotion including recreational such as dancing, and constitute a significant portion of a person's mass. Female legs generally have greater hip anteversion and tibiofemoral angles, but shorter femur and tibial lengths than those in males.
Spasticity is a feature of altered skeletal muscle performance with a combination of paralysis, increased tendon reflex activity, and hypertonia. It is also colloquially referred to as an unusual "tightness", stiffness, or "pull" of muscles.

The sciatic nerve, also called the ischiadic nerve, is a large nerve in humans and other vertebrate animals which is the largest branch of the sacral plexus and runs alongside the hip joint and down the lower limb. It is the longest and widest single nerve in the human body, going from the top of the leg to the foot on the posterior aspect. The sciatic nerve has no cutaneous branches for the thigh. This nerve provides the connection to the nervous system for the skin of the lateral leg and the whole foot, the muscles of the back of the thigh, and those of the leg and foot. It is derived from spinal nerves L4 to S3. It contains fibers from both the anterior and posterior divisions of the lumbosacral plexus.

The cauda equina is a bundle of spinal nerves and spinal nerve rootlets, consisting of the second through fifth lumbar nerve pairs, the first through fifth sacral nerve pairs, and the coccygeal nerve, all of which arise from the lumbar enlargement and the conus medullaris of the spinal cord. The cauda equina occupies the lumbar cistern, a subarachnoid space inferior to the conus medullaris. The nerves that compose the cauda equina innervate the pelvic organs and lower limbs to include motor innervation of the hips, knees, ankles, feet, internal anal sphincter and external anal sphincter. In addition, the cauda equina extends to sensory innervation of the perineum and, partially, parasympathetic innervation of the bladder.

Sciatica is pain going down the leg from the lower back. This pain may go down the back, outside, or front of the leg. Onset is often sudden following activities like heavy lifting, though gradual onset may also occur. The pain is often described as shooting. Typically, symptoms are only on one side of the body. Certain causes, however, may result in pain on both sides. Lower back pain is sometimes present. Weakness or numbness may occur in various parts of the affected leg and foot.
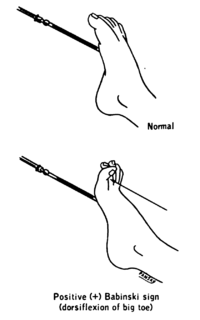
The plantar reflex is a reflex elicited when the sole of the foot is stimulated with a blunt instrument. The reflex can take one of two forms. In healthy adults, the plantar reflex causes a downward response of the hallux (flexion). An upward response (extension) of the hallux is known as the Babinski response or Babinski sign, named after the neurologist Joseph Babinski. The presence of the Babinski sign can identify disease of the spinal cord and brain in adults, and also exists as a primitive reflex in infants.

A reflex arc is a neural pathway that controls a reflex. In vertebrates, most sensory neurons do not pass directly into the brain, but synapse in the spinal cord. This allows for faster reflex actions to occur by activating spinal motor neurons without the delay of routing signals through the brain. The brain will receive the input while the reflex is being carried out and the analysis of the signal takes place after the reflex action.
Clonus is a set of involuntary and rhythmic muscular contractions and relaxations. Clonus is a sign of certain neurological conditions, particularly associated with upper motor neuron lesions involving descending motor pathways, and in many cases is, accompanied by spasticity. Unlike small, spontaneous twitches known as fasciculations, clonus causes large motions that are usually initiated by a reflex. Studies have shown clonus beat frequency to range from three to eight Hz on average, and may last a few seconds to several minutes depending on the patient’s condition.

Cauda equina syndrome (CES) is a condition that occurs when the bundle of nerves below the end of the spinal cord known as the cauda equina is damaged. Signs and symptoms include low back pain, pain that radiates down the leg, numbness around the anus, and loss of bowel or bladder control. Onset may be rapid or gradual.
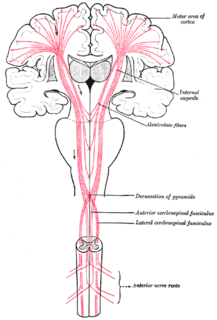
An upper motor neuron lesion Is an injury or abnormality that occurs in the neural pathway above the anterior horn cell of the spinal cord or motor nuclei of the cranial nerves. Conversely, a lower motor neuron lesion affects nerve fibers traveling from the anterior horn of the spinal cord or the cranial motor nuclei to the relevant muscle(s).

A nerve conduction study (NCS) is a medical diagnostic test commonly used to evaluate the function, especially the ability of electrical conduction, of the motor and sensory nerves of the human body. These tests may be performed by medical specialists such as clinical neurophysiologists, physical therapists, chiropractors, physiatrists, and neurologists who subspecialize in electrodiagnostic medicine. In the United States, neurologists and physiatrists receive training in electrodiagnostic medicine as part of residency training and in some cases acquire additional expertise during a fellowship in clinical neurophysiology, electrodiagnostic medicine, or neuromuscular medicine. Outside the US, clinical neurophysiologists learn needle EMG and NCS testing.

The gastrocnemius muscle is a superficial two-headed muscle that is in the back part of the lower leg of humans. It runs from its two heads just above the knee to the heel, a three joint muscle. The muscle is named via Latin, from Greek γαστήρ (gaster) 'belly' or 'stomach' and κνήμη (knḗmē) 'leg', meaning 'stomach of leg'.

The plantaris is one of the superficial muscles of the superficial posterior compartment of the leg, one of the fascial compartments of the leg.

Foot drop is a gait abnormality in which the dropping of the forefoot happens due to weakness, irritation or damage to the deep fibular nerve, including the sciatic nerve, or paralysis of the muscles in the anterior portion of the lower leg. It is usually a symptom of a greater problem, not a disease in itself. Foot drop is characterized by inability or impaired ability to raise the toes or raise the foot from the ankle (dorsiflexion). Foot drop may be temporary or permanent, depending on the extent of muscle weakness or paralysis and it can occur in one or both feet. In walking, the raised leg is slightly bent at the knee to prevent the foot from dragging along the ground.
The sural nerve is a sensory nerve in the calf region of the leg. It is made up of branches of the tibial nerve and common fibular nerve, the medial cutaneous branch from the tibial nerve, and the lateral cutaneous branch from the common fibular nerve. Once formed, the nerves runs down the mid calf to the ankle and along the skin from the mid-posterior popliteal fossa to just behind to the lateral malleolus and then under the malleolus and forward along the lateral aspect of the foot.

The stretch reflex, or more accurately "muscle stretch reflex", is a muscle contraction in response to stretching within the muscle. The reflex functions to maintain the muscle at a constant length. The term deep tendon reflex is often wrongfully used by many health workers and students to refer to this reflex. "Tendons have little to do with the response, other than being responsible for mechanically transmitting the sudden stretch from the reflex hammer to the muscle spindle. In addition, some muscles with stretch reflexes have no tendons ".
Hyporeflexia refers to below normal or absent reflexes (areflexia). It can be detected through the use of a reflex hammer. It is the opposite of hyperreflexia. Hyporeflexia is generally associated with a lower motor neuron deficit, whereas hyperreflexia is often attributed to upper motor neuron lesions. The upper motor neurons are thought to inhibit the reflex arc, which is formed by sensory neurons from intrafusal fibers of muscles, lower motor neurons and appurtenant interneurons. Therefore, damage to lower motor neurons will subsequently result in hyporeflexia and/or areflexia.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, numbness, or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.
References
- ↑ "Medscape- Neurologic examination" . Retrieved 6 February 2013.
- ↑ Walker, HK (1990). "Deep Tendon Reflexes". In Walker, HK; Hall, WD; Hurst, JW (eds.). Clinical Methods: The History, Physical, and Laboratory Examinations (3 ed.). Boston: Butterworths. Retrieved 18 July 2017.
- ↑ William J. Weiner (30 July 2010). Neurology for the Non-Neurologist. Lippincott Williams & Wilkins. pp. 499–. ISBN 978-1-60547-239-3 . Retrieved 4 July 2011.
- ↑ "Diagnosis". Archived from the original on 9 June 2014. Retrieved 6 February 2013.