Involuntary commitment, civil commitment, involuntary hospitalization or involuntary hospitalisation, is a legal process through which an individual who is deemed by a qualified agent to have symptoms of severe mental disorder is detained in a psychiatric hospital (inpatient) where they can be treated involuntarily. This treatment may involve the administration of psychoactive drugs, including involuntary administration. In many jurisdictions, people diagnosed with mental health disorders can also be forced to undergo treatment while in the community; this is sometimes referred to as outpatient commitment and shares legal processes with commitment.
Outpatient commitment—also called assisted outpatient treatment (AOT) or community treatment orders (CTO)—refers to a civil court procedure wherein a legal process orders an individual diagnosed with a severe mental disorder to adhere to an outpatient treatment plan designed to prevent further deterioration or recurrence that is harmful to themselves or others.

Psychiatric hospitals, also known as mental health units or behavioral health units, are hospitals or wards specializing in the treatment of severe mental disorders, such as schizophrenia, bipolar disorder, and major depressive disorder. Psychiatric hospitals vary widely in their size and grading. Some hospitals may specialize only in short-term or outpatient therapy for low-risk patients. Others may specialize in the temporary or permanent containment of patients who need routine assistance, treatment, or a specialized and controlled environment due to a psychiatric disorder. Patients often choose voluntary commitment, but those whom psychiatrists believe to pose significant danger to themselves or others may be subject to involuntary commitment and involuntary treatment. Psychiatric hospitals may also be called psychiatric wards/units when they are a subunit of a regular hospital.
The Lanterman–Petris–Short (LPS) Act regulates involuntary civil commitment to a mental health institution in the state of California. The act set the precedent for modern mental health commitment procedures in the United States. The bipartisan bill was co-authored by California State Assemblyman Frank D. Lanterman (R) and California State Senators Nicholas C. Petris (D) and Alan Short (D), and signed into law in 1967 by Governor Ronald Reagan. The Act went into full effect on July 1, 1972. It cited seven articles of intent:
Laura's Law is a California state law that allows for court-ordered assisted outpatient treatment. To qualify for the program, the person must have a serious mental illness plus a recent history of psychiatric hospitalizations, jailings or acts, threats or attempts of serious violent behavior towards self or others. A complete functional outline of the legal procedures and safeguards within Laura's Law has been prepared by NAMI San Mateo.

Emergency psychiatry is the clinical application of psychiatry in emergency settings. Conditions requiring psychiatric interventions may include attempted suicide, substance abuse, depression, psychosis, violence or other rapid changes in behavior. Psychiatric emergency services are rendered by professionals in the fields of medicine, nursing, psychology and social work. The demand for emergency psychiatric services has rapidly increased throughout the world since the 1960s, especially in urban areas. Care for patients in situations involving emergency psychiatry is complex.

The Mental Health Act 1983 (c.20) is an Act of the Parliament of the United Kingdom. It covers the reception, care and treatment of mentally disordered people, the management of their property and other related matters, forming part of the mental health law for the people in England and Wales. In particular, it provides the legislation by which people diagnosed with a mental disorder can be detained in a hospital or police custody and have their disorder assessed or treated against their wishes, informally known as "sectioning". Its use is reviewed and regulated by the Care Quality Commission. The Act was significantly amended by the Mental Health Act 2007. A white paper proposing changes to the act was published in 2021 following an independent review of the act by Simon Wessely.
Involuntary treatment refers to medical treatment undertaken without the consent of the person being treated. Involuntary treatment is permitted by law in some countries when overseen by the judiciary through court orders; other countries defer directly to the medical opinions of doctors.
Kendra's Law, effective since November 1999, is a New York State law concerning involuntary outpatient commitment also known as assisted outpatient treatment. It grants judges the authority to issue orders that require people who meet certain criteria to regularly undergo psychiatric treatment. Failure to comply could result in commitment for up to 72 hours. Kendra's Law does not mandate that patients be forced to take medication.

Castle Peak Hospital is the oldest psychiatric hospital in Hong Kong. Located at the east of Castle Peak in Tuen Mun, the hospital was established in 1961. Currently, it has 1,156 beds, providing a wide variety of psychiatric services such as adult psychiatry, forensic psychiatry, psychogeriatric services, child and adolescent psychiatry, consultation-liaison psychiatry and substance abuse treatments. All wards in the hospital are equipped to accommodate both voluntary and involuntary admitted patients.

Deinstitutionalisation is the process of replacing long-stay psychiatric hospitals with less isolated community mental health services for those diagnosed with a mental disorder or developmental disability. In the late 20th century, it led to the closure of many psychiatric hospitals, as patients were increasingly cared for at home, in halfway houses and clinics, in regular hospitals, or not at all.
The psychiatric survivors movement is a diverse association of individuals who either currently access mental health services, or who are survivors of interventions by psychiatry.
The Florida Mental Health Act of 1971, commonly known as the "Baker Act," allows the involuntary institutionalization and examination of an individual.
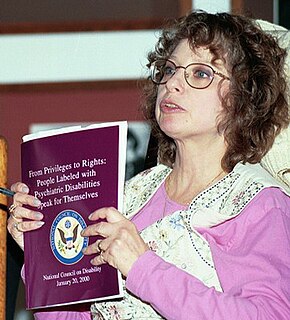
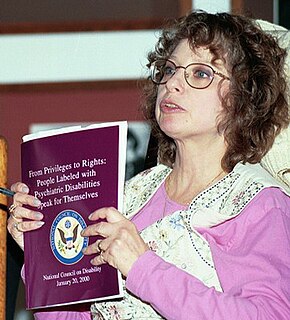
Judi Chamberlin was an American activist, leader, organizer, public speaker and educator in the psychiatric survivors movement. Her political activism followed her involuntary confinement in a psychiatric facility in the 1960s. She was the author of On Our Own: Patient-Controlled Alternatives to the Mental Health System, which is a foundational text in the Mad Pride movement.
The obligatory dangerousness criterion is a principle present in the mental health law of many developed countries. It mandates evidence of dangerousness to oneself or to others before involuntary treatment for mental illness. The term “dangerousness” refers to one’s ability to hurt oneself or others physically or mentally within an imminent time frame, and the harm caused must have a long-term effect on the person(s).

Mental health in Russia is covered by a law, known under its official name—the Law of the Russian Federation "On Psychiatric Care and Guarantees of Citizens' Rights during Its Provision", which is the basic legal act that regulates psychiatric care in the Russian Federation and applies not only to persons with mental disorders but all citizens. A notable exception of this rule is those vested with parliamentary or judicial immunity. Providing psychiatric care is regulated by a special law regarding guarantees of citizens' rights.
Involuntary commitment or civil commitment is a legal process through which an individual with symptoms of severe mental illness is court-ordered into treatment in a hospital (inpatient) or in the community (outpatient).
A high-dependency unit (HDU) is an inpatient psychiatric ward, typically with only a small number of beds, attached to an acute admissions ward. It is intended to provide treatment for patients who cannot be managed safely on an acute (open) ward, but do not meet the threshold for admission to PICU. The number of staff per patient will be higher than the associated acute ward, but may be lower than levels at a PICU.
The United States has experienced two waves of deinstitutionalization, the process of replacing long-stay psychiatric hospitals with less isolated community mental health services for those diagnosed with a mental disorder or developmental disability.
Independent mental health advocacy, IMHA, is advocacy for someone being treated, possibly involuntarily, for a mental disorder provided by someone not involved in the treatment. IMHA can help a service user understand and exercise their rights and ensure their views and preferences are expressed. Advocacy seeks to address unequal power relations between mental health professionals and those using their services. Those who provide such advocacy are called Independent mental health advocates, IMHA.