Orthopedic surgery or orthopedics is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors, and congenital disorders.
An osteotomy is a surgical operation whereby a bone is cut to shorten or lengthen it or to change its alignment. It is sometimes performed to correct a hallux valgus, or to straighten a bone that has healed crookedly following a fracture. It is also used to correct a coxa vara, genu valgum, and genu varum. The operation is done under a general anaesthetic.

Hip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant, that is, a hip prosthesis. Hip replacement surgery can be performed as a total replacement or a hemi/semi(half) replacement. Such joint replacement orthopaedic surgery is generally conducted to relieve arthritis pain or in some hip fractures. A total hip replacement consists of replacing both the acetabulum and the femoral head while hemiarthroplasty generally only replaces the femoral head. Hip replacement is one of the most common orthopaedic operations, though patient satisfaction varies widely. Approximately 58% of total hip replacements are estimated to last 25 years. The average cost of a total hip replacement in 2012 was $40,364 in the United States, and about $7,700 to $12,000 in most European countries.

Avascular necrosis (AVN), also called osteonecrosis or bone infarction, is death of bone tissue due to interruption of the blood supply. Early on, there may be no symptoms. Gradually joint pain may develop, which may limit the person's ability to move. Complications may include collapse of the bone or nearby joint surface.
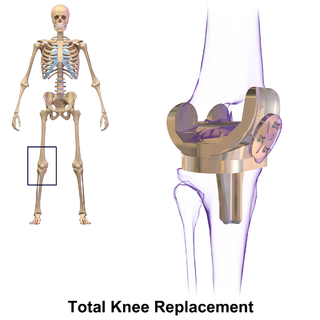
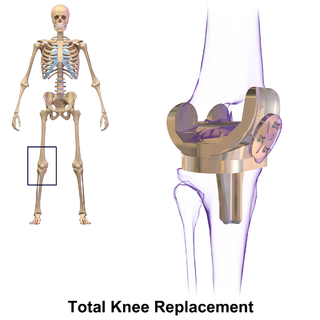
Knee replacement, also known as knee arthroplasty, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability, most commonly offered when joint pain is not diminished by conservative sources. It may also be performed for other knee diseases, such as rheumatoid arthritis. In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long-standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation, and is not a reason to perform knee replacement.

Joint replacement is a procedure of orthopedic surgery known also as arthroplasty, in which an arthritic or dysfunctional joint surface is replaced with an orthopedic prosthesis. Joint replacement is considered as a treatment when severe joint pain or dysfunction is not alleviated by less-invasive therapies. Joint replacement surgery is often indicated from various joint diseases, including osteoarthritis and rheumatoid arthritis.

Hip resurfacing has been developed as a surgical alternative to total hip replacement (THR). The procedure consists of placing a cap, which is hollow and shaped like a mushroom, over the head of the femur while a matching metal cup is placed in the acetabulum, replacing the articulating surfaces of the person's hip joint and removing very little bone compared to a THR. When the person moves the hip, the movement of the joint induces synovial fluid to flow between the hard metal bearing surfaces lubricating them when the components are placed in the correct position. The surgeon's level of experience with hip resurfacing is most important; therefore, the selection of the right surgeon is crucial for a successful outcome. Health-related quality of life measures are markedly improved and the person's satisfaction is favorable after hip resurfacing arthroplasty.

Hip dysplasia is an abnormality of the hip joint where the socket portion does not fully cover the ball portion, resulting in an increased risk for joint dislocation. Hip dysplasia may occur at birth or develop in early life. Regardless, it does not typically produce symptoms in babies less than a year old. Occasionally one leg may be shorter than the other. The left hip is more often affected than the right. Complications without treatment can include arthritis, limping, and low back pain. Females are affected more often than males. Risk factors for hip dysplasia include female sex, family history, certain swaddling practices, and breech presentation whether an infant is delivered vaginally or by cesarean section. If one identical twin is affected, there is a 40% risk the other will also be affected. Screening all babies for the condition by physical examination is recommended. Ultrasonography may also be useful.

Unicompartmental knee arthroplasty (UKA) is a surgical procedure used to relieve arthritis in one of the knee compartments in which the damaged parts of the knee are replaced. UKA surgery may reduce post-operative pain and have a shorter recovery period than a total knee replacement procedure, particularly in people over 75 years of age. Moreover, UKAs may require a smaller incision, less tissue damage, and faster recovery times.
Minimally invasive hip resurfacing (MIS) is a total or partial hip surgery that can be carried out through an incision of less than 10 cm without imparting great forces on the anatomy or compromising component positioning.
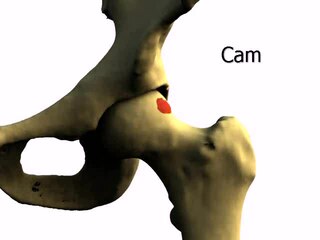
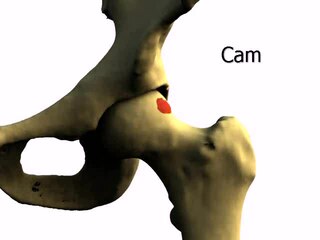
Femoroacetabular impingement (FAI) is a condition involving one or more anatomical abnormalities of the hip joint, which is a ball and socket joint. It is a common cause of hip pain and discomfort in young and middle-aged adults. It occurs when the ball shaped femoral head contacts the acetabulum abnormally or does not permit a normal range of motion in the acetabular socket. Damage can occur to the articular cartilage, or labral cartilage, or both. The condition may be symptomatic or asymptomatic. It may cause osteoarthritis of the hip. Treatment options range from conservative management to surgery.
"Professor" Derek McMinn is a British orthopaedic surgeon and inventor who practised in Birmingham, United Kingdom at the BMI Edgbaston Hospital until his suspension in 2020. McMinn is currently under police investigation for allegedly keeping the body parts of thousands of patients over a 25-year period.
Michael J. Bronson is an American orthopaedic surgeon who is Chairman of the Department of Orthopedic Surgery, Mount Sinai West and Mount Sinai Morningside, and Chief of Joint Replacement Surgery at the Icahn School of Medicine at Mount Sinai in New York, and the author of advances in the development of minimally invasive surgical instruments to advance unicondylar partial knee replacement, including the Vision Total Hip System, a widely used hip replacement system that avoids the use of cement.
Metallosis is the medical condition involving deposition and build-up of metal debris in the soft tissues of the body.

Hip arthroscopy refers to the viewing of the interior of the acetabulofemoral (hip) joint through an arthroscope and the treatment of hip pathology through a minimally invasive approach. This technique is sometimes used to help in the treatment of various joint disorders and has gained popularity because of the small incisions used and shorter recovery times when compared with conventional surgical techniques. Hip arthroscopy was not feasible until recently, new technology in both the tools used and the ability to distract the hip joint has led to a recent surge in the ability to do hip arthroscopy and the popularity of it.
Limb-sparing techniques, also known as limb-saving or limb-salvage techniques, are performed in order to preserve the look and function of limbs. Limb-sparing techniques are used to preserve limbs affected by trauma, arthritis, cancers such as high-grade bone sarcomas, and vascular conditions such as diabetic foot ulcers. As the techniques for chemotherapy, radiation, and diagnostic modalities improve, there has been a trend toward limb-sparing procedures to avoid amputation, which has been associated with a lower 5-year survival rate and cost-effectiveness compared to limb salvage in the long-run. There are many different types of limb-sparing techniques, including arthrodesis, arthroplasty, endoprosthetic reconstruction, various types of implants, rotationplasty, osseointegration limb replacement, fasciotomy, and revascularization.

After hip replacement, hip prosthesis zones are regions in the interface between prosthesis material and the surrounding bone. These are used as reference regions when describing for example complications including hip prosthesis loosening on medical imaging. Postoperative controls after hip replacement surgery is routinely done by projectional radiography in anteroposterior and lateral views.

Labral reconstruction is a type of hip arthroscopy in which the patient's native labrum is partially or completely removed and reconstructed using either autograft or allograft tissue. Originally described in 2009 using the ligamentum teres capitis, arthroscopic labral reconstruction using a variety of graft tissue has demonstrated promising short and mid-term clinical outcomes. Most importantly, labral reconstruction has demonstrated utility when the patient's native labral tissue is far too damaged for debridement or repair.

Reverse shoulder replacement is a type of shoulder replacement in which the normal ball and socket relationship of glenohumeral joint is reversed, creating a more stable joint with a fixed fulcrum. This form of shoulder replacement is utilized in situations in which conventional shoulder replacement surgery would lead to poor outcomes and high failure rates.
Dr. Javad Parvizi is an American Board Certified orthopaedic surgeon and the director of clinical research at the Rothman Orthopaedic Institute, Philadelphia. He holds the James Edwards Professor Chair of Orthopaedics at Thomas Jefferson University. He is the co-founder of the International Consensus Meeting and President of the Musculoskeletal Infection Society (MSIS).