Related Research Articles

The superior vena cava (SVC) is the superior of the two venae cavae, the great venous trunks that return deoxygenated blood from the systemic circulation to the right atrium of the heart. It is a large-diameter (24 mm) short length vein that receives venous return from the upper half of the body, above the diaphragm. Venous return from the lower half, below the diaphragm, flows through the inferior vena cava. The SVC is located in the anterior right superior mediastinum. It is the typical site of central venous access via a central venous catheter or a peripherally inserted central catheter. Mentions of "the cava" without further specification usually refer to the SVC.

Pulmonary heart disease, also known as cor pulmonale, is the enlargement and failure of the right ventricle of the heart as a response to increased vascular resistance or high blood pressure in the lungs.
Kussmaul's sign is a paradoxical rise in jugular venous pressure (JVP) on inspiration, or a failure in the appropriate fall of the JVP with inspiration. It can be seen in some forms of heart disease and is usually indicative of limited right ventricular filling due to right heart dysfunction.

The jugular venous pressure is the indirectly observed pressure over the venous system via visualization of the internal jugular vein. It can be useful in the differentiation of different forms of heart and lung disease. Classically three upward deflections and two downward deflections have been described.

The jugular veins are veins that take deoxygenated blood from the head back to the heart via the superior vena cava. The internal jugular vein descends next to the internal carotid artery and continues posteriorly to the sternocleidomastoid muscle.
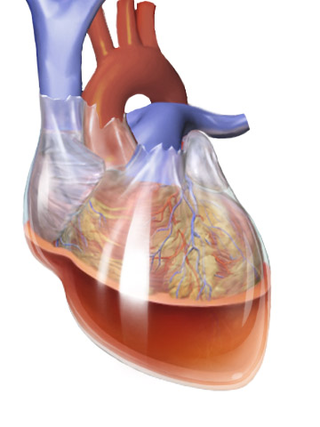
Beck's triad is a collection of three medical signs associated with acute cardiac tamponade, a medical emergency when excessive fluid accumulates in the pericardial sac around the heart and impairs its ability to pump blood. The signs are low arterial blood pressure, distended neck veins, and distant, muffled heart sounds.

The atrium is one of two upper chambers in the heart that receives blood from the circulatory system. The blood in the atria is pumped into the heart ventricles through the atrioventricular valves.

A pulmonary artery catheter (PAC), also known as a Swan-Ganz catheter or right heart catheter, is a balloon-tipped catheter that is inserted into a pulmonary artery in a procedure known as pulmonary artery catheterization or right heart catheterization. Pulmonary artery catheterization is a useful measure of the overall function of the heart particularly in those with complications from heart failure, heart attack, arrythmias or pulmonary embolism. It is also a good measure for those needing intravenous fluid therapy, for instance post heart surgery, shock, and severe burns. The procedure can also be used to measure pressures in the heart chambers.
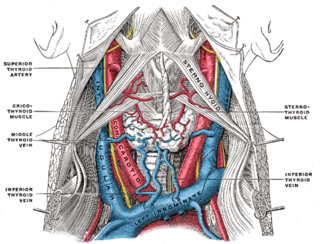
The internal jugular vein is a paired jugular vein that collects blood from the brain and the superficial parts of the face and neck. This vein runs in the carotid sheath with the common carotid artery and vagus nerve.
In medicine, the cardiac examination, also precordial exam, is performed as part of a physical examination, or when a patient presents with chest pain suggestive of a cardiovascular pathology. It would typically be modified depending on the indication and integrated with other examinations especially the respiratory examination.

Transjugular intrahepatic portosystemic shunt is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein. It is used to treat portal hypertension which frequently leads to intestinal bleeding, life-threatening esophageal bleeding and the buildup of fluid within the abdomen (ascites).
Traumatic asphyxia, or Perthes's syndrome, is a medical emergency caused by an intense compression of the thoracic cavity, causing venous back-flow from the right side of the heart into the veins of the neck and the brain.

Right ventricular hypertrophy (RVH) is a condition defined by an abnormal enlargement of the cardiac muscle surrounding the right ventricle. The right ventricle is one of the four chambers of the heart. It is located towards the lower-end of the heart and it receives blood from the right atrium and pumps blood into the lungs.
In medicine, Friedreich's sign is the exaggerated drop in diastolic central venous pressure seen in constrictive pericarditis and manifested as abrupt collapse of the neck veins or marked descent of the central venous pressure waveform. The normal jugular venous waveform contains two descents, x and y. The x descent, which corresponds to the combination of right atrial relaxation and depression of the atrial floor during ventricular contraction, is normally dominant. The y descent occurs as a result of passive ventricular filling during early diastole and is usually absent in patients with tamponade. In constrictive pericarditis, the characteristic sharp and deep y descent reflects rapid filling in early diastole which occurs when the unyielding pericardium elevates atrial pressure and limits ventricular filling to the early diastolic period. Friedreich’s diastolic collapse of the cervical veins, describes a sharp and deep y descent of the jugular venous waveform. It can be a clue to the diagnosis of constrictive pericarditis.

Chronic venous insufficiency (CVI) is a medical condition in which blood pools in the veins, straining the walls of the vein. The most common cause of CVI is superficial venous reflux which is a treatable condition. As functional venous valves are required to provide for efficient blood return from the lower extremities, this condition typically affects the legs. If the impaired vein function causes significant symptoms, such as swelling and ulcer formation, it is referred to as chronic venous disease. It is sometimes called chronic peripheral venous insufficiency and should not be confused with post-thrombotic syndrome in which the deep veins have been damaged by previous deep vein thrombosis.
Obstructive shock is one of the four types of shock, caused by a physical obstruction in the flow of blood. Obstruction can occur at the level of the great vessels or the heart itself. Causes include pulmonary embolism, cardiac tamponade, and tension pneumothorax. These are all life-threatening. Symptoms may include shortness of breath, weakness, or altered mental status. Low blood pressure and tachycardia are often seen in shock. Other symptoms depend on the underlying cause.

Pacemaker syndrome is a condition that represents the clinical consequences of suboptimal atrioventricular (AV) synchrony or AV dyssynchrony, regardless of the pacing mode, after pacemaker implantation. It is an iatrogenic disease—an adverse effect resulting from medical treatment—that is often underdiagnosed. In general, the symptoms of the syndrome are a combination of decreased cardiac output, loss of atrial contribution to ventricular filling, loss of total peripheral resistance response, and nonphysiologic pressure waves.
The cardiovascular examination is a portion of the physical examination that involves evaluation of the cardiovascular system. The exact contents of the examination will vary depending on the presenting complaint but a complete examination will involve the heart, lungs, belly and the blood vessels.

Heart failure with preserved ejection fraction (HFpEF) is a form of heart failure in which the ejection fraction – the percentage of the volume of blood ejected from the left ventricle with each heartbeat divided by the volume of blood when the left ventricle is maximally filled – is normal, defined as greater than 50%; this may be measured by echocardiography or cardiac catheterization. Approximately half of people with heart failure have preserved ejection fraction, while the other half have a reduction in ejection fraction, called heart failure with reduced ejection fraction (HFrEF).

Bernheim Syndrome is a presumed disorder whereby the right ventricle is severely compressed due to a shift in the ventricular septal wall of the heart leading to heart failure. It was first described by Hippolyte Bernheim in 1910. Today it is questioned whether or not Bernheim Syndrome is its own syndrome or a side effect of other cardiac conditions such as left ventricular heart failure whereby the left ventricle is substantially enlarged which encroaches on the space of the right ventricle.
References
- 1 2 Wiese, J. (July 2000). "The abdominojugular reflux sign". American Journal of Medicine . 109 (1): 59–61. doi:10.1016/s0002-9343(00)00443-5. PMID 10936479.
- 1 2 3 4 Ewy G (1988). "The abdominojugular test: technique and hemodynamic correlates". Annals of Internal Medicine . 109 (6): 456–60. doi:10.7326/0003-4819-109-6-456. PMID 3415106.
- ↑ Elsevier, Dorland's Illustrated Medical Dictionary, Elsevier.
- 1 2 Cook D, Simel D (1996). "The Rational Clinical Examination. Does this patient have abnormal central venous pressure?". JAMA. 275 (8): 630–4. doi:10.1001/jama.1996.03530320054034. PMID 8594245.
- ↑ Marantz P, Kaplan M, Alderman M (1990). "Clinical diagnosis of congestive heart failure in patients with acute dyspnea". Chest. 97 (4): 776–81. doi:10.1378/chest.97.4.776. PMID 2182296.