Related Research Articles

In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

The tibia, also known as the shinbone or shankbone, is the larger, stronger, and anterior (frontal) of the two bones in the leg below the knee in vertebrates ; it connects the knee with the ankle. The tibia is found on the medial side of the leg next to the fibula and closer to the median plane. The tibia is connected to the fibula by the interosseous membrane of leg, forming a type of fibrous joint called a syndesmosis with very little movement. The tibia is named for the flute tibia. It is the second largest bone in the human body, after the femur. The leg bones are the strongest long bones as they support the rest of the body.

The posterior cruciate ligament (PCL) is a ligament in each knee of humans and various other animals. It works as a counterpart to the anterior cruciate ligament (ACL). It connects the posterior intercondylar area of the tibia to the medial condyle of the femur. This configuration allows the PCL to resist forces pushing the tibia posteriorly relative to the femur.

The anterior cruciate ligament (ACL) is one of a pair of cruciate ligaments in the human knee. The two ligaments are called "cruciform" ligaments, as they are arranged in a crossed formation. In the quadruped stifle joint, based on its anatomical position, it is also referred to as the cranial cruciate ligament. The term cruciate is Latin for cross. This name is fitting because the ACL crosses the posterior cruciate ligament to form an "X". It is composed of strong, fibrous material and assists in controlling excessive motion by limiting mobility of the joint. The anterior cruciate ligament is one of the four main ligaments of the knee, providing 85% of the restraining force to anterior tibial displacement at 30 and 90° of knee flexion. The ACL is the most frequently injured ligament in the knee.

The Segond fracture is a type of avulsion fracture from the lateral tibial plateau of the knee, immediately below the articular surface of the tibia.
The drawer test is used in the initial clinical assessment of suspected rupture of the cruciate ligaments in the knee.

The medial meniscus is a fibrocartilage semicircular band that spans the knee joint medially, located between the medial condyle of the femur and the medial condyle of the tibia. It is also referred to as the internal semilunar fibrocartilage. The medial meniscus has more of a crescent shape while the lateral meniscus is more circular. The anterior aspects of both menisci are connected by the transverse ligament. It is a common site of injury, especially if the knee is twisted.

The lateral meniscus is a fibrocartilaginous band that spans the lateral side of the interior of the knee joint. It is one of two menisci of the knee, the other being the medial meniscus. It is nearly circular and covers a larger portion of the articular surface than the medial. It can occasionally be injured or torn by twisting the knee or applying direct force, as seen in contact sports.
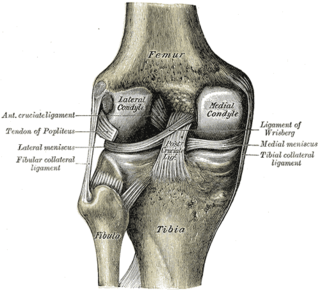
The lower extremity of femur is the lower end of the femur in human and other animals, closer to the knee. It is larger than the upper extremity of femur, is somewhat cuboid in form, but its transverse diameter is greater than its antero-posterior; it consists of two oblong eminences known as the lateral condyle and medial condyle.

Cruciate ligaments are pairs of ligaments arranged like a letter X. They occur in several joints of the body, such as the knee joint, wrist joint and the atlanto-axial joint. In a fashion similar to the cords in a toy Jacob's ladder, the crossed ligaments stabilize the joint while allowing a very large range of motion.

The unhappy triad, also known as a blown knee among other names, is an injury to the anterior cruciate ligament, medial collateral ligament, and meniscus. Analysis during the 1990s indicated that this 'classic' O'Donoghue triad is actually an unusual clinical entity among athletes with knee injuries. Some authors mistakenly believe that in this type of injury, "combined anterior cruciate and medial collateral ligament disruptions that were incurred during athletic endeavors" always present with concomitant medial meniscus injury. However, the 1990 analysis showed that lateral meniscus tears are more common than medial meniscus tears in conjunction with sprains of the ACL.

The articular capsule of the knee joint is the wide and lax joint capsule of the knee. It is thin in front and at the side, and contains the patella, ligaments, menisci, and bursae of the knee. The capsule consists of an inner synovial membrane, and an outer fibrous membrane separated by fatty deposits anteriorly and posteriorly.

A tear of a meniscus is a rupturing of one or more of the fibrocartilage strips in the knee called menisci. When doctors and patients refer to "torn cartilage" in the knee, they actually may be referring to an injury to a meniscus at the top of one of the tibiae. Menisci can be torn during innocuous activities such as walking or squatting. They can also be torn by traumatic force encountered in sports or other forms of physical exertion. The traumatic action is most often a twisting movement at the knee while the leg is bent. In older adults, the meniscus can be damaged following prolonged 'wear and tear'. Especially acute injuries can lead to displaced tears which can cause mechanical symptoms such as clicking, catching, or locking during motion of the joint. The joint will be in pain when in use, but when there is no load, the pain goes away.
The pivot-shift test is one of the three major tests for assessing anterior cruciate injury or laxity, the other two being the anterior drawer and Lachman test. However, unlike the other two, it tests for instability, an important determinant as to how the knee will function. In fact, it is instability, not simply the injury to the anterior cruciate ligament itself, that places the menisci at future risk, and gives rise to the feeling that the "knee is not secure" or "may give out".

A patellar dislocation is a knee injury in which the patella (kneecap) slips out of its normal position. Often the knee is partly bent, painful and swollen. The patella is also often felt and seen out of place. Complications may include a patella fracture or arthritis.

Knee pain is pain in or around the knee.
Posterolateral corner injuries of the knee are injuries to a complex area formed by the interaction of multiple structures. Injuries to the posterolateral corner can be debilitating to the person and require recognition and treatment to avoid long term consequences. Injuries to the PLC often occur in combination with other ligamentous injuries to the knee; most commonly the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL). As with any injury, an understanding of the anatomy and functional interactions of the posterolateral corner is important to diagnosing and treating the injury.

A tibial plateau fracture is a break of the upper part of the tibia (shinbone) that involves the knee joint. This could involve the medial, lateral, central, or bicondylar. Symptoms include pain, swelling, and a decreased ability to move the knee. People are generally unable to walk. Complication may include injury to the artery or nerve, arthritis, and compartment syndrome.

Medial knee injuries are the most common type of knee injury. The medial ligament complex of the knee consists of:

The function of the posterior cruciate ligament (PCL) is to prevent the femur from sliding off the anterior edge of the tibia and to prevent the tibia from displacing posterior to the femur. Common causes of PCL injuries are direct blows to the flexed knee, such as the knee hitting the dashboard in a car accident or falling hard on the knee, both instances displacing the tibia posterior to the femur.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 Teresa L., Schraeder; Richard M., Terek; C. Christopher, Smith (22 July 2010). "Clinical Evaluation of the Knee". The New England Journal of Medicine. 363 (4): 5. doi:10.1056/NEJMvcm0803821. PMID 20660399.
- ↑ Cimino, Francesca; Volk, Bradford Scott; Setter, Don (2010-10-15). "Anterior cruciate ligament injury: diagnosis, management, and prevention". American Family Physician. 82 (8): 917–922. ISSN 1532-0650. PMID 20949884.
- ↑ Jacobs, Brian (21 March 2011). "eMedicine – Knee Osteochondritis Dissecans". Mediscape. Retrieved 2 April 2011.
- ↑ Wittke R (November 2004). "Acute and chronic injuries to the knee in the doctor's office". MMW Fortschr Med (in German). 146 (45): 46–49. PMID 15581106.