In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.
Tendinopathy is a type of tendon disorder that results in pain, swelling, and impaired function. The pain is typically worse with movement. It most commonly occurs around the shoulder, elbow, wrist, hip, knee, or ankle.

A sprain is a soft tissue injury of the ligaments within a joint, often caused by a sudden movement abruptly forcing the joint to exceed its functional range of motion. Ligaments are tough, inelastic fibers made of collagen that connect two or more bones to form a joint and are important for joint stability and proprioception, which is the body's sense of limb position and movement. Sprains may be mild, moderate, or severe, with the latter two classes involving some degree of tearing of the ligament. Sprains can occur at any joint but most commonly occur in the ankle, knee, or wrist. An equivalent injury to a muscle or tendon is known as a strain.

Tennis elbow, also known as lateral epicondylitis or enthesopathy of the extensor carpi radialis origin, is an enthesopathy of the origin of the extensor carpi radialis brevis on the lateral epicondyle. The outer part of the elbow becomes painful and tender. The pain may also extend into the back of the forearm. Onset of symptoms is generally gradual, although they can seem sudden and be misinterpreted as an injury. Golfer's elbow is a similar condition that affects the inside of the elbow.

Osgood–Schlatter disease (OSD) is inflammation of the patellar ligament at the tibial tuberosity (apophysitis) usually affecting adolescents during growth spurts. It is characterized by a painful bump just below the knee that is worse with activity and better with rest. Episodes of pain typically last a few weeks to months. One or both knees may be affected and flares may recur.

Chondromalacia patellae is an inflammation of the underside of the patella and softening of the cartilage.

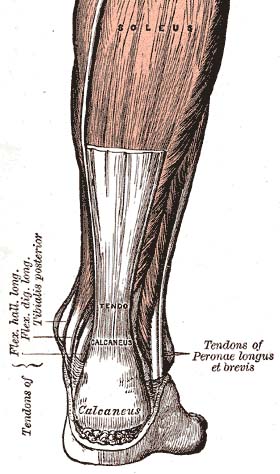
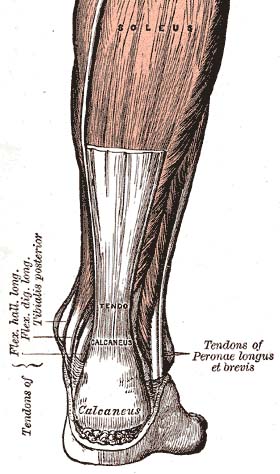
The plantaris is one of the superficial muscles of the superficial posterior compartment of the leg, one of the fascial compartments of the leg.
Snapping hip syndrome, also referred to as dancer's hip, is a medical condition characterized by a snapping sensation felt when the hip is flexed and extended. This may be accompanied by a snapping or popping noise and pain or discomfort. Pain often decreases with rest and diminished activity. Snapping hip syndrome is commonly classified by the location of the snapping as either extra-articular or intra-articular.

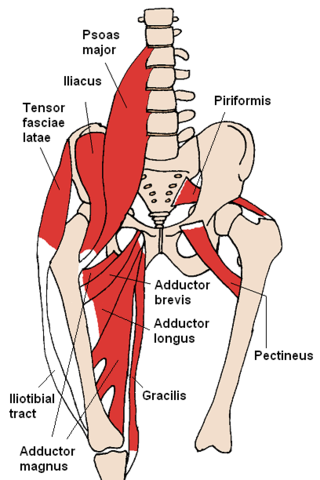
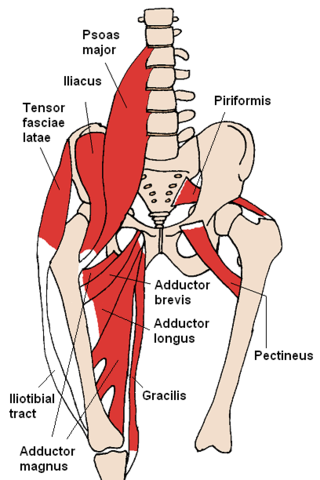
The iliotibial tract or iliotibial band is a longitudinal fibrous reinforcement of the fascia lata. The action of the muscles associated with the ITB flex, extend, abduct, and laterally and medially rotate the hip. The ITB contributes to lateral knee stabilization. During knee extension the ITB moves anterior to the lateral condyle of the femur, while ~30 degrees knee flexion, the ITB moves posterior to the lateral condyle. However, it has been suggested that this is only an illusion due to the changing tension in the anterior and posterior fibers during movement. It originates at the anterolateral iliac tubercle portion of the external lip of the iliac crest and inserts at the lateral condyle of the tibia at Gerdy's tubercle. The figure shows only the proximal part of the iliotibial tract.
The knee examination, in medicine and physiotherapy, is performed as part of a physical examination, or when a patient presents with knee pain or a history that suggests a pathology of the knee joint.

Knee taping is a procedure performed by physiotherapists or physicians to alleviate the symptoms of patellofemoral pain. Though knee taping has been shown to offer short-term pain relief, its long-term efficacy is confounded by several studies. The mechanism of action by which it alleviates pain is unknown, though it has been suggested by physicians that it could correct patella position, facilitate/inhibit quadriceps components or bear stress associated with peripatellar tissues or patellar compression. Evidence for these suggestions, however, has been contradictory or absent.
Greater trochanteric pain syndrome (GTPS), a form of bursitis, is inflammation of the trochanteric bursa, a part of the hip.

Patellofemoral pain syndrome is knee pain as a result of problems between the kneecap and the femur. The pain is generally in the front of the knee and comes on gradually. Pain may worsen with sitting, excessive use, or climbing and descending stairs.
Patellar subluxation syndrome, is an injury that is concerned with the kneecap. Patellar subluxation is more common than patellar dislocation and is just as disabling.

A patellar dislocation is a knee injury in which the patella (kneecap) slips out of its normal position. Often the knee is partly bent, painful and swollen. The patella is also often felt and seen out of place. Complications may include a patella fracture or arthritis.
The medial patellofemoral ligament (MPFL) is one of several ligaments on the medial aspect of the knee. It originates in the superomedial aspect of the patella and inserts in the space between the adductor tubercle and the medial femoral epicondyle. The ligament itself extends from the femur to the superomedial patella, and its shape is similar to a trapezoid. It keeps the patella in place, but its main function is to prevent lateral displacement of the patella.

Knee pain is pain in or around the knee.

Medial knee injuries are the most common type of knee injury. The medial ligament complex of the knee consists of:
Muscle strain is one of the most common injuries in tennis. When an isolated large-energy appears during the muscle contraction and at the same time, bodyweight applies huge amounts of pressure to the lengthened muscle, which can result in the occurrence of muscle strain. Inflammation and bleeding are triggered when muscle strain occur which resulted in redness, pain and swelling. Overuse is also common in tennis players from all levels. Muscle, cartilage, nerves, bursae, ligaments and tendons may be damaged from overuse. The repetitive use of a particular muscle without time for repair and recover in the most common case among the injury.
Running injuries affect about half of runners annually. The frequencies of various RRI depend on the type of running, such as speed and mileage. Some injuries are acute, caused by sudden overstress, such as side stitch, strains, and sprains. Many of the common injuries that affect runners are chronic, developing over longer periods as the result of overuse. Common overuse injuries include shin splints, stress fractures, Achilles tendinitis, Iliotibial band syndrome, Patellofemoral pain, and plantar fasciitis.