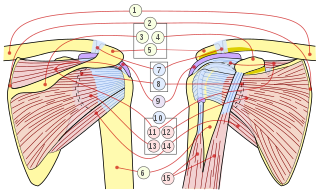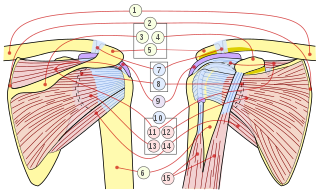
The rotator cuff is a group of muscles and their tendons that act to stabilize the human shoulder and allow for its extensive range of motion. Of the seven scapulohumeral muscles, four make up the rotator cuff. The four muscles are:
Tendinopathy is a type of tendon disorder that results in pain, swelling, and impaired function. The pain is typically worse with movement. It most commonly occurs around the shoulder, elbow, wrist, hip, knee, or ankle.

Shoulder problems including pain, are one of the more common reasons for physician visits for musculoskeletal symptoms. The shoulder is the most movable joint in the body. However, it is an unstable joint because of the range of motion allowed. This instability increases the likelihood of joint injury, often leading to a degenerative process in which tissues break down and no longer function well.

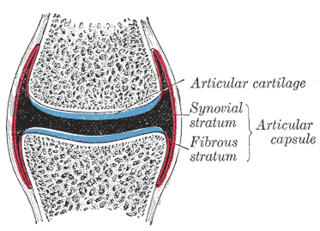
Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone. It is believed to be the fourth leading cause of disability in the world, affecting 1 in 7 adults in the United States alone. The most common symptoms are joint pain and stiffness. Usually the symptoms progress slowly over years. Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs, the knee and hip joints, and the joints of the neck and lower back. The symptoms can interfere with work and normal daily activities. Unlike some other types of arthritis, only the joints, not internal organs, are affected.

Plantar fasciitis or plantar heel pain is a disorder of the plantar fascia, which is the connective tissue that supports the arch of the foot. It results in pain in the heel and bottom of the foot that is usually most severe with the first steps of the day or following a period of rest. Pain is also frequently brought on by bending the foot and toes up towards the shin. The pain typically comes on gradually, and it affects both feet in about one-third of cases.

Tennis elbow, also known as lateral epicondylitis or enthesopathy of the extensor carpi radialis origin, is an enthesopathy of the origin of the extensor carpi radialis brevis on the lateral epicondyle. The outer part of the elbow becomes painful and tender. The pain may also extend into the back of the forearm. Onset of symptoms is generally gradual, although they can seem sudden and be misinterpreted as an injury. Golfer's elbow is a similar condition that affects the inside of the elbow.

Piriformis syndrome is a condition which is believed to result from nerve compression at the sciatic nerve by the piriformis muscle. It is a specific case of deep gluteal syndrome. The largest and most bulky nerve in the human body is the sciatic nerve. Starting at its origin it is 2 cm wide and 0.5 cm thick. The sciatic nerve forms the roots of L4-S3 segments of the lumbosacral plexus. The nerve will pass inferiorly to the piriformis muscle, in the direction of the lower limb where it divides into common tibial and fibular nerves. Symptoms may include pain and numbness in the buttocks and down the leg. Often symptoms are worsened with sitting or running.
Rotator cuff tendinopathy is a process of senescence. The pathophysiology is mucoid degeneration. Most people develop rotator cuff tendinopathy within their lifetime.

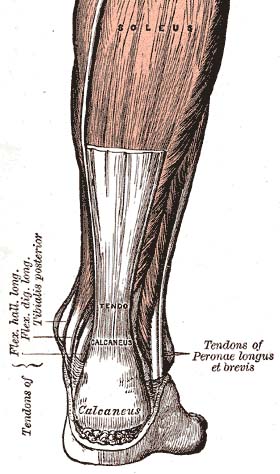
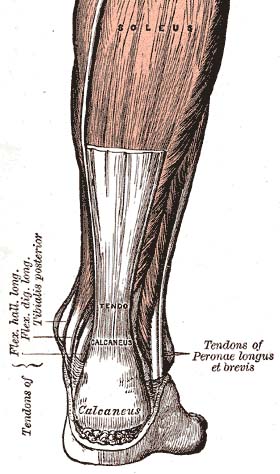
Achilles tendon rupture is when the Achilles tendon, at the back of the ankle, breaks. Symptoms include the sudden onset of sharp pain in the heel. A snapping sound may be heard as the tendon breaks and walking becomes difficult.

An enthesopathy refers to a disorder involving the attachment of a tendon or ligament to a bone. This site of attachment is known as the enthesis . If the condition is known to be inflammatory, it can more precisely be called an enthesitis.

Morton's neuroma is a benign neuroma of an intermetatarsal plantar nerve, most commonly of the second and third intermetatarsal spaces, which results in the entrapment of the affected nerve. The main symptoms are pain and/or numbness, sometimes relieved by ceasing to wear footwear with tight toe boxes and high heels. The condition is named after Thomas George Morton, though it was first correctly described by a chiropodist named Durlacher.
Greater trochanteric pain syndrome (GTPS), a form of bursitis, is inflammation of the trochanteric bursa, a part of the hip.

Subacromial bursitis is a condition caused by inflammation of the bursa that separates the superior surface of the supraspinatus tendon from the overlying coraco-acromial ligament, acromion, and coracoid and from the deep surface of the deltoid muscle. The subacromial bursa helps the motion of the supraspinatus tendon of the rotator cuff in activities such as overhead work.

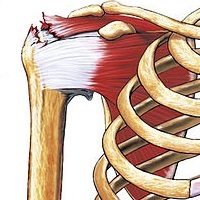
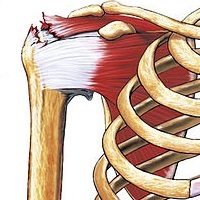
Calcific tendinitis is a common condition where deposits of calcium phosphate form in a tendon, sometimes causing pain at the affected site. Deposits can occur in several places in the body, but are by far most common in the rotator cuff of the shoulder. Around 80% of those with deposits experience symptoms, typically chronic pain during certain shoulder movements, or sharp acute pain that worsens at night. Calcific tendinitis is typically diagnosed by physical exam and X-ray imaging. The disease often resolves completely on its own, but is typically treated with non-steroidal anti-inflammatory drugs to relieve pain, rest and physical therapy to promote healing, and in some cases various procedures to breakdown and/or remove the calcium deposits.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, altered sensation (paresthesia) or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.

Extracorporeal shockwave therapy (ESWT) is a treatment using powerful acoustic pulses which is mostly used to treat kidney stones and in physical therapy and orthopedics.
Arthrofibrosis has been described in most joints like knee, hip, ankle, foot joints, shoulder, elbow, wrist, hand joints as well as spinal vertebrae. It can occur after injury or surgery or may arise without an obvious cause. There is excessive scar tissue formation within the joint and/or surrounding soft tissues leading to painful restriction of joint motion that persists despite physical therapy and rehabilitation. The scar tissue may be located inside the knee joint or may involve the soft tissue structures around the knee joint, or both locations.

The capsule of the glenohumeral (shoulder) joint is the articular capsule of the shoulder. It completely surrounds the joint. It is attached above to the circumference of the glenoid cavity beyond the glenoidal labrum, and below to the anatomical neck of the humerus, approaching nearer to the articular cartilage above than in the rest of its extent.
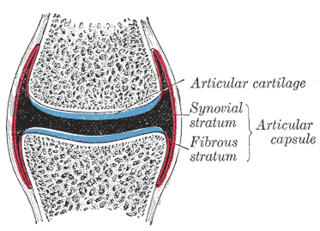
In anatomy, capsulitis is inflammation of a capsule.

Shoulder impingement syndrome is a syndrome involving tendonitis of the rotator cuff muscles as they pass through the subacromial space, the passage beneath the acromion. It is particularly associated with tendonitis of the supraspinatus muscle. This can result in pain, weakness, and loss of movement at the shoulder.