Iliotibial band syndrome (ITBS) is the second most common knee injury, and is caused by inflammation located on the lateral aspect of the knee due to friction between the iliotibial band and the lateral epicondyle of the femur. Pain is felt most commonly on the lateral aspect of the knee and is most intensive at 30 degrees of knee flexion. Risk factors in women include increased hip adduction and knee internal rotation. Risk factors seen in men are increased hip internal rotation and knee adduction. ITB syndrome is most associated with long-distance running, cycling, weight-lifting, and with military training.

In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

Shoulder problems including pain, are one of the more common reasons for physician visits for musculoskeletal symptoms. The shoulder is the most movable joint in the body. However, it is an unstable joint because of the range of motion allowed. This instability increases the likelihood of joint injury, often leading to a degenerative process in which tissues break down and no longer function well.

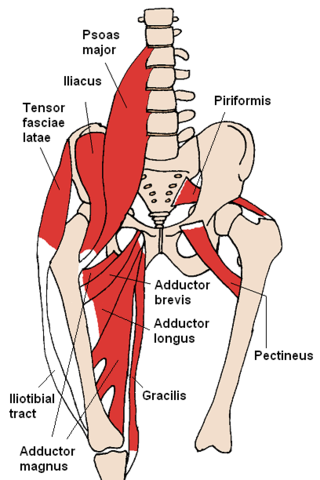
The gluteus maximus is the main extensor muscle of the hip in humans. It is the largest and outermost of the three gluteal muscles and makes up a large part of the shape and appearance of each side of the hips. It is the single largest muscle in the human body. Its thick fleshy mass, in a quadrilateral shape, forms the prominence of the buttocks. The other gluteal muscles are the medius and minimus, and sometimes informally these are collectively referred to as the glutes.

The gluteus medius, one of the three gluteal muscles, is a broad, thick, radiating muscle. It is situated on the outer surface of the pelvis.

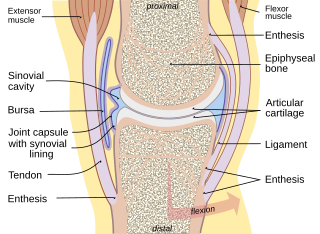
Bursitis is the inflammation of one or more bursae of synovial fluid in the body. They are lined with a synovial membrane that secretes a lubricating synovial fluid. There are more than 150 bursae in the human body. The bursae rest at the points where internal functionaries, such as muscles and tendons, slide across bone. Healthy bursae create a smooth, almost frictionless functional gliding surface making normal movement painless. When bursitis occurs, however, movement relying on the inflamed bursa becomes difficult and painful. Moreover, movement of tendons and muscles over the inflamed bursa aggravates its inflammation, perpetuating the problem. Muscle can also be stiffened.
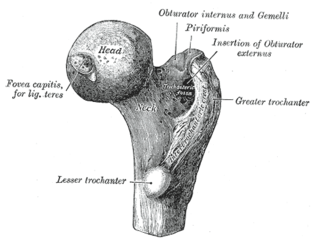
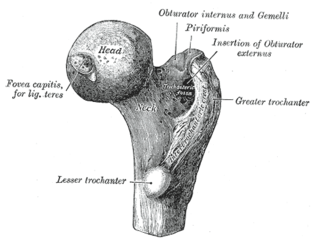
The greater trochanter of the femur is a large, irregular, quadrilateral eminence and a part of the skeletal system.

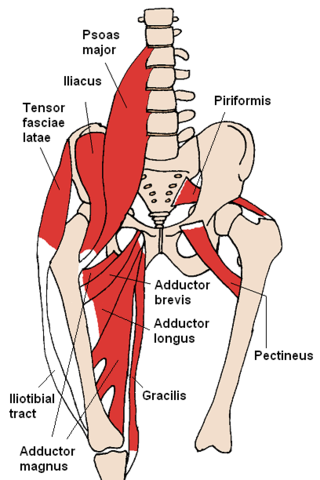
The piriformis muscle is a flat, pyramidally-shaped muscle in the gluteal region of the lower limbs. It is one of the six muscles in the lateral rotator group.

Piriformis syndrome is a condition which is believed to result from compression of the sciatic nerve by the piriformis muscle. The largest and most bulky nerve in the human body is the sciatic nerve. Starting at its origin it is 2 cm wide and 0.5 cm thick. The sciatic nerve forms the roots of L4-S3 segments of the lumbosacral plexus. The nerve will pass inferiorly to the piriformis muscle, in the direction of the lower limb where it divides into common tibial and fibular nerves. Symptoms may include pain and numbness in the buttocks and down the leg. Often symptoms are worsened with sitting or running.
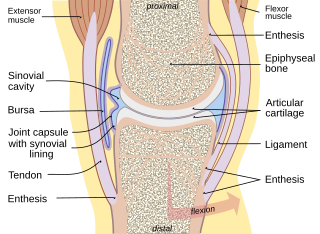
A synovial bursa, usually simply bursa, is a small fluid-filled sac lined by synovial membrane with an inner capillary layer of viscous synovial fluid. It provides a cushion between bones and tendons and/or muscles around a joint. This helps to reduce friction between the bones and allows free movement. Bursae are found around most major joints of the body.

The internal obturator muscle or obturator internus muscle originates on the medial surface of the obturator membrane, the ischium near the membrane, and the rim of the pubis.

The tensor fasciae latae is a muscle of the thigh. Together with the gluteus maximus, it acts on the iliotibial band and is continuous with the iliotibial tract, which attaches to the tibia. The muscle assists in keeping the balance of the pelvis while standing, walking, or running.

The gluteal muscles, often called glutes, are a group of three muscles which make up the gluteal region commonly known as the buttocks: the gluteus maximus, gluteus medius and gluteus minimus. The three muscles originate from the ilium and sacrum and insert on the femur. The functions of the muscles include extension, abduction, external rotation, and internal rotation of the hip joint.
Trendelenburg gait, named after Friedrich Trendelenburg, is an abnormal gait. It is caused by weakness or ineffective action of the gluteus medius muscle and the gluteus minimus muscle.
Snapping hip syndrome, also referred to as dancer's hip, is a medical condition characterized by a snapping sensation felt when the hip is flexed and extended. This may be accompanied by a snapping or popping noise and pain or discomfort. Pain often decreases with rest and diminished activity. Snapping hip syndrome is commonly classified by the location of the snapping as either extra-articular or intra-articular.
A bursectomy is the removal of a bursa, which is a small sac filled with synovial fluid that cushions adjacent bone structures and reduces friction in joint movement. This procedure is usually carried out to relieve chronic inflammation (bursitis) or infection, when conservative management has failed to improve patient outcomes.

Subacromial bursitis is a condition caused by inflammation of the bursa that separates the superior surface of the supraspinatus tendon from the overlying coraco-acromial ligament, acromion, and coracoid and from the deep surface of the deltoid muscle. The subacromial bursa helps the motion of the supraspinatus tendon of the rotator cuff in activities such as overhead work.

Extracorporeal shockwave therapy (ESWT) is a non-invasive, out-patient alternative to surgery for those with many joint and tendon disorders. ESWT sends acoustic shock waves into bone or soft tissue, in effect reinjuring the area on a cellular level and breaking up the scarring that has penetrated tendons and ligaments. The controlled reinjuring of tissue allows the body to regenerate blood vessels and bone cells. The resulting revascularization leads to faster healing and often a return to pre-injury activity levels. ESWT is mostly used for kidney stones removal, in physical therapy and orthopedics.

Pes anserine bursitis is an inflammatory condition of the medial (inner) knee at the anserine bursa, a sub muscular bursa, just below the pes anserinus.

Knee pain is pain in or around the knee.