Cherry angioma, also called cherry hemangioma or Campbell de Morgan Spot, is a small bright red dome-shaped bump on the skin. It ranges between 0.5 – 6 mm in diameter and usually several are present, typically on the chest and arms, and increasing in number with age. If scratched, they may bleed.
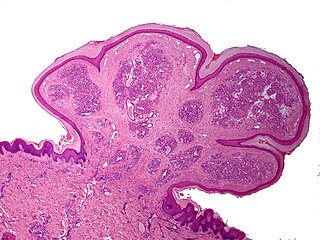
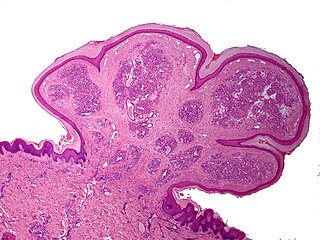
A pyogenic granuloma or lobular capillary hemangioma is a vascular tumor that occurs on both mucosa and skin, and appears as an overgrowth of tissue due to irritation, physical trauma, or hormonal factors. It is often found to involve the gums, skin, or nasal septum, and has also been found far from the head, such as in the thigh.

Focal nodular hyperplasia is a benign tumor of the liver, which is the second most prevalent tumor of the liver after hepatic hemangioma. It is usually asymptomatic, rarely grows or bleeds, and has no malignant potential. This tumour was once often resected because it was difficult to distinguish from hepatic adenoma, but with modern multiphase imaging it is usually now diagnosed by strict imaging criteria and not resected.

A vascular tumor is a tumor of vascular origin; a soft tissue growth that can be either benign or malignant, formed from blood vessels or lymph vessels. Examples of vascular tumors include hemangiomas, lymphangiomas, hemangioendotheliomas, Kaposi's sarcomas, angiosarcomas, and hemangioblastomas. An angioma refers to any type of benign vascular tumor.

Amelanotic melanoma is a type of skin cancer in which the cells do not make any melanin. They can be pink, red, purple or of normal skin color, and are therefore difficult to diagnose correctly. They can occur anywhere on the body, just as a typical melanoma can.

Kimura's disease is a benign rare chronic inflammatory disorder. Its primary symptoms are subdermal lesions in the head or neck or painless unilateral inflammation of cervical lymph nodes.
Lupus erythematosus panniculitis presents with subcutaneous nodules that are commonly firm, sharply defined and nontender.
Anetoderma is a benign but uncommon disorder that causes localized areas of flaccid or herniated sac-like skin due to a focal reduction of dermal elastic tissue. Anetoderma is subclassified as primary anetoderma, secondary anetoderma, iatrogenic anetoderma of prematurity, congenital anetoderma, familial anetoderma, and drug-induced anetoderma.
Palisaded neutrophilic and granulomatous dermaititis (PNGS) is usually associated with a well-defined connective tissue disease, lupus erythematosus or rheumatoid arthritis most commonly, and often presents with eroded or ulcerated symmetrically distributed umbilicated papules or nodules on the elbows.

Chondrodermatitis nodularis chronica helicis(CNCH) is a small, nodular, tender, chronic inflammatory lesion occurring on the helix of the ear, most often in men. it often presents as a benign painful erythematous nodule fixed to the cartilage of the helix or antihelix of the external ear. Although the exact cause of the condition is unknown, it has been linked to head pressure on the ear while sleeping. Treatment options include the use of pressure-relieving devices or, in cases where that is not an option, surgery.

Linear IgA bullous dermatosis is a rare immune-mediated blistering skin disease frequently associated with medication exposure, especially vancomycin, with men and women being equally affected. It was first described by Tadeusz Chorzelski in 1979 and may be divided into two types:
Neutrophilic dermatosis of the dorsal hands (NDDH) is a skin condition that presents with edematous pustular or ulcerative nodules or plaques localized to the dorsal hands.
Self-healing juvenile cutaneous mucinosis is a skin condition caused by fibroblasts producing abnormally large amounts of mucopolysaccharides, and is characterized by the sudden onset of skin lesions and polyarthritis.

Trigeminal trophic syndrome is a rare disease caused by the interruption of peripheral or central sensory pathways of the trigeminal nerve. A slowly enlarging, uninflammed ulcer can occur in the area that has had trigeminal nerve damage; including but not limited to the cheek beside the ala nasi.

Generalized granuloma annulare is a skin condition of unknown cause, tending to affect women in the fifth and sixth decades, presenting as a diffuse but symmetrical, papular or annular eruption of more than ten skin lesions, and often hundreds.

Pagetoid reticulosis is a cutaneous condition, an uncommon lymphoproliferative disorder, sometimes considered a form of mycosis fungoides.
Primary cutaneous anaplastic large cell lymphoma belongs to the group of cutaneous processes that are CD30+ lymphoproliferative and are characterized by autoregressive, recurrent, single or multifocal ulcerating nodules. Single or localized nodules, papules, or plaques are present in the majority of patients. However, a patient may have more than one lesion in up to 20% of cases.

Airbag dermatitis is skin irritation secondary to the deployment of airbags. The diagnosis of "air bag dermatitis" is relatively recent; the first case was reported in 1994.
Rheumatoid neutrophilic dermatitis, also known as rheumatoid neutrophilic dermatosis, is a cutaneous condition associated with rheumatoid arthritis.
IgG4-related skin disease is the recommended name for skin manifestations in IgG4-related disease (IgG4-RD). Multiple different skin manifestations have been described.