Neutropenia is an abnormally low concentration of neutrophils in the blood. Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteria, bacterial fragments and immunoglobulin-bound viruses in the blood. People with neutropenia are more susceptible to bacterial infections and, without prompt medical attention, the condition may become life-threatening.

Eosinophilia is a condition in which the eosinophil count in the peripheral blood exceeds 5×108/L (500/μL). Hypereosinophilia is an elevation in an individual's circulating blood eosinophil count above 1.5 × 109/L (i.e. 1,500/μL). The hypereosinophilic syndrome is a sustained elevation in this count above 1.5 × 109/L (i.e. 1,500/μL) that is also associated with evidence of eosinophil-based tissue injury.
Leukocytosis is a condition in which the white cell (leukocyte) count is above the normal range in the blood. It is frequently a sign of an inflammatory response, most commonly the result of infection, but may also occur following certain parasitic infections or bone tumors as well as leukemia. It may also occur after strenuous exercise, convulsions such as epilepsy, emotional stress, pregnancy and labor, anesthesia, as a side effect of medication, and epinephrine administration. There are five principal types of leukocytosis:
- Neutrophilia
- Lymphocytosis
- Monocytosis
- Eosinophilia
- Basophilia

Cryoglobulinemia is a medical condition in which the blood contains large amounts of pathological cold sensitive antibodies called cryoglobulins – proteins that become insoluble at reduced temperatures. This should be contrasted with cold agglutinins, which cause agglutination of red blood cells.

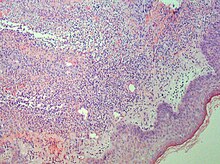
Pyoderma gangrenosum is a rare, inflammatory skin disease where painful pustules or nodules become ulcers that progressively grow. Pyoderma gangrenosum is not infectious.
Fever of unknown origin (FUO) refers to a condition in which the patient has an elevated temperature (fever) but, despite investigations by one or more qualified physicians, no explanation is found.

A promyelocyte is a granulocyte precursor, developing from the myeloblast and developing into the myelocyte. Promyelocytes measure 12–20 microns in diameter. The nucleus of a promyelocyte is approximately the same size as a myeloblast but their cytoplasm is much more abundant. They also have less prominent nucleoli than myeloblasts and their chromatin is more coarse and clumped. The cytoplasm is basophilic and contains primary red/purple granules.
A genital ulcer is an open sore located on the genital area, which includes the vulva, penis, perianal region, or anus. Genital ulcers are most commonly caused by infectious agents. However, this is not always the case, as a genital ulcer may have noninfectious causes as well.
Chronic recurrent multifocal osteomyelitis (CRMO) is a rare condition (1:1,000,000), in which the bones have lesions, inflammation, and pain. It is called multifocal because it can appear in different parts of the body, primarily bones, and osteomyelitis because it is very similar to that disease, although CRMO appears to be without any infection.
Neutrophilic eccrine hidradenitis (NEH) usually is a cutaneous complication of chemotherapy, but it can also occur for other reasons. It consists of fever and non specific skin lesions. It is rare, and self-limited.

Acute generalized exanthematous pustulosis (AGEP) is a rare skin reaction that in 90% of cases is related to medication.
Reactive neutrophilic dermatoses are a spectrum of conditions mediated by neutrophils, and typically associated with underlying diseases, such as inflammatory bowel disease and hematologic malignancy.
Neutrophilic dermatosis of the dorsal hands (NDDH) is a skin condition that presents with edematous pustular or ulcerative nodules or plaques localized to the dorsal hands.
Behçet's disease is recognized as a disease that cause inflammatory perivasculitis, inflammation of the tissue around a blood or lymph vessel, in practically any tissue in the body. Usually, prevalent symptoms include canker sores or ulcers in the mouth and on the genitals, and inflammation in parts of the eye. In addition, patients experience severe headache and papulopustular skin lesions as well. The disease was first described in 1937 by a Turkish dermatologist, Dr. Hulusi Behçet. Behçet's disease is most prevalent in the Middle East and the Far East regions; however, it is rare in America regions.

White blood cells, also called immune cells or immunocytes, are cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. White blood cells include three main subtypes: granulocytes, lymphocytes and monocytes.

Bowel-associated dermatosis–arthritis syndrome (BADAS), is a complication of jejunoileal bypass surgery consisting of flu-like symptoms, multiple painful joints (polyarthralgia), muscle aches (myalgia) and skin changes. It has been reported to occur in up to 20% of patients who had jejunoileal bypass surgery, a form of obesity surgery that is rarely performed today.

Behçet's disease (BD) is a type of inflammatory disorder which affects multiple parts of the body. The most common symptoms include painful sores on the mucous membranes of the mouth and other parts of the body, inflammation of parts of the eye, and arthritis. The sores can last from a few days, up to a week or more. Less commonly there may be inflammation of the brain or spinal cord, blood clots, aneurysms, or blindness. Often, the symptoms come and go.
Cutaneous manifestations of COVID-19 are characteristic signs or symptoms of the Coronavirus disease 2019 that occur in the skin. The American Academy of Dermatology reports that skin lesions such as morbilliform, pernio, urticaria, macular erythema, vesicular purpura, papulosquamous purpura and retiform purpura are seen in people with COVID-19. Pernio-like lesions were more common in mild disease while retiform purpura was seen only in critically ill patients. The major dermatologic patterns identified in individuals with COVID-19 are urticarial rash, confluent erythematous/morbilliform rash, papulovesicular exanthem, chilbain-like acral pattern, livedo reticularis and purpuric "vasculitic" pattern. Chilblains and Multisystem inflammatory syndrome in children are also cutaneous manifestations of COVID-19.
Autoinflammatory diseases (AIDs) are a group of rare disorders caused by dysfunction of the innate immune system. These responses are characterized by periodic or chronic systemic inflammation, usually without the involvement of adaptive immunity.