Related Research Articles
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender. The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals. It is also known as sex reassignment surgery, gender confirmation surgery, and several other names.

Hypospadias is a common variation in fetal development of the penis in which the urethra does not open from its usual location on the head of the penis. It is the second-most common birth defect of the male reproductive system, affecting about one of every 250 males at birth. Roughly 90% of cases are the less serious distal hypospadias, in which the urethral opening is on or near the head of the penis (glans). The remainder have proximal hypospadias, in which the meatus is all the way back on the shaft of the penis, near or within the scrotum. Shiny tissue that typically forms the urethra instead extends from the meatus to the tip of the glans; this tissue is called the urethral plate.

Chordee is a condition in which the head of the penis curves downward or upward, at the junction of the head and shaft of the penis. The curvature is usually most obvious during erection, but resistance to straightening is often apparent in the flaccid state as well. In many cases but not all, chordee is associated with hypospadias. This is not the same condition as Peyronie's disease, which involves curvature of the shaft of the penis most commonly due to injury during adult life.
Phalloplasty is the construction or reconstruction of a penis or the artificial modification of the penis by surgery. The term is also occasionally used to refer to penis enlargement.

Metoidioplasty, metaoidioplasty, or metaidoioplasty is a female-to-male gender-affirming surgery.
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning.
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.
Vaginoplasty is any surgical procedure that results in the construction or reconstruction of the vagina. It is a type of genitoplasty. Pelvic organ prolapse is often treated with one or more surgeries to repair the vagina. Sometimes a vaginoplasty is needed following the treatment or removal of malignant growths or abscesses to restore a normal vaginal structure and function. Surgery to the vagina is done to correct congenital defects to the vagina, urethra and rectum. It may correct protrusion of the urinary bladder into the vagina (cystocele) and protrusion of the rectum (rectocele) into the vagina. Often, a vaginoplasty is performed to repair the vagina and its attached structures due to trauma or injury.

Intersex medical interventions (IMI), also known as intersex genital mutilations (IGM), are surgical, hormonal and other medical interventions performed to modify atypical or ambiguous genitalia and other sex characteristics, primarily for the purposes of making a person's appearance more typical and to reduce the likelihood of future problems. The history of intersex surgery has been characterized by controversy due to reports that surgery can compromise sexual function and sensation, and create lifelong health issues. The medical interventions can be for a variety of reasons, due to the enormous variety of the disorders of sex development. Some disorders, such as salt-wasting disorder, can be life-threatening if left untreated.

The history of intersex surgery is intertwined with the development of the specialities of pediatric surgery, pediatric urology, and pediatric endocrinology, with our increasingly refined understanding of sexual differentiation, with the development of political advocacy groups united by a human qualified analysis, and in the last decade by doubts as to efficacy, and controversy over when and even whether some procedures should be performed.

Bladder exstrophy is a congenital anomaly that exists along the spectrum of the exstrophy-epispadias complex, and most notably involves protrusion of the urinary bladder through a defect in the abdominal wall. Its presentation is variable, often including abnormalities of the bony pelvis, pelvic floor, and genitalia. The underlying embryologic mechanism leading to bladder exstrophy is unknown, though it is thought to be in part due to failed reinforcement of the cloacal membrane by underlying mesoderm. Exstrophy means the inversion of a hollow organ.

Scrotoplasty, also known as oscheoplasty, is a type of surgery to create or repair the scrotum. The history of male genital plastic surgery is rooted in many cultures and dates back to ancient times. However, scientific research for male genital plastic surgery such as scrotoplasty began to develop in the early 1900s. The development of testicular implants began in 1940 made from materials outside of what is used today. Today, testicular implants are created from saline or gel filled silicone rubber. There are a variety of reasons why scrotoplasty is done. Some transgender men and intersex or non-binary people who were assigned female at birth may choose to have this surgery to create a scrotum, as part of their transition. Other reasons for this procedure include addressing issues with the scrotum due to birth defects, aging, or medical conditions such as infection. For newborn males with penoscrotal defects such as webbed penis, a condition in which the penile shaft is attached to the scrotum, scrotoplasty can be performed to restore normal appearance and function. For older male adults, the scrotum may extend with age. Scrotoplasty or scrotal lift can be performed to remove the loose, excess skin. Scrotoplasty can also be performed for males who undergo infection, necrosis, traumatic injury of the scrotum.

Partial androgen insensitivity syndrome (PAIS) is a condition that results in the partial inability of the cell to respond to androgens. It is an X linked recessive condition. The partial unresponsiveness of the cell to the presence of androgenic hormones impairs the masculinization of male genitalia in the developing fetus, as well as the development of male secondary sexual characteristics at puberty, but does not significantly impair female genital or sexual development. As such, the insensitivity to androgens is clinically significant only when it occurs in individuals with a Y chromosome. Clinical features include ambiguous genitalia at birth and primary amenhorrhoea with clitoromegaly with inguinal masses. Müllerian structures are not present in the individual.

A penile implant is an implanted device intended for the treatment of erectile dysfunction, Peyronie's disease, ischemic priapism, deformity and any traumatic injury of the penis, and for phalloplasty or metoidioplasty, including in gender-affirming surgery. Men also opt for penile implants for aesthetic purposes. Men's satisfaction and sexual function is influenced by discomfort over genital size which leads to seek surgical and non-surgical solutions for penis alteration. Although there are many distinct types of implants, most fall into one of two categories: malleable and inflatable transplants.

Disorders of sex development (DSDs), also known as differences in sex development or variations in sex characteristics (VSC), are congenital conditions affecting the reproductive system, in which development of chromosomal, gonadal, or anatomical sex is atypical.

A micropenis is an unusually small penis. A common criterion is a dorsal penile length of at least 2.5 standard deviations smaller than the mean human penis size. A micropenis is stretched penile length equal to or less than 1.9 cm in term infants, and 9.3 cm in adults. The condition is usually recognized shortly after birth. The term is most often used medically when the rest of the penis, scrotum, and perineum are without ambiguity, such as hypospadias. A microphallus describes a medical term where other sections of genitallia are different, such as hypospadias or cryptorchidism. Micropenis incidence is about 1.5 in 10,000 male newborns in North America.
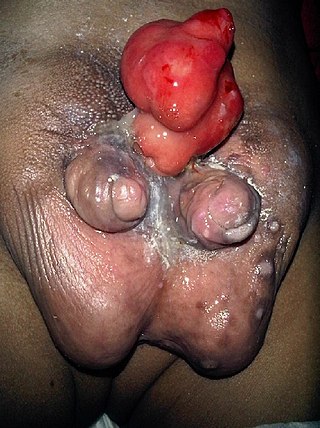
Diphallia, penile duplication (PD), diphallic terata, or diphallasparatus is an extremely rare developmental abnormality in which a male is born with two penises. The first reported case was by Johannes Jacob Wecker in 1609. Its occurrence is 1 in 5.5 million boys in the United States.

Buried penis, also called hidden penis or retractile penis, is a congenital or acquired condition in which the penis is partially or completely hidden below the surface of the skin. A buried penis can lead to urinary difficulties, poor hygiene, infection, and inhibition of normal sexual function.

Webbed penis also known as buried or concealed penis is an acquired or congenital condition in which the scrotal skin extends onto the ventral penile shaft. The penile shaft is buried in the scrotum or tethered to the scrotal midline by a fold or web of skin. The urethra and erectile bodies are usually normal. Webbed penis is usually asymptomatic, but the cosmetic appearance is often unacceptable. This condition may be corrected by surgical techniques.
Male genital examination is a physical examination of the genital in males to detect ailments and to assess sexual development, and is normally a component of an annual physical examination. The examination includes checking the penis, scrotum, and urethral meatus. A comprehensive assessment of the male genitals assesses the pubic hair based on Sexual Maturity Rating and the size of the testicles and penis. The exam can also be conducted to verify a person's age and biological sex. The genitourinary system can also be assessed as part of the male genital examination. During a genital examination, the doctor can detect any of the following: structural abnormalities, urethral opening abnormalities, problems related to not being circumcised, lumps, tumors, redness, excoriation, edema, lesions, swelling, cancer, hair-related issues, and many others. In some instances where a physical examination of the male genitals is not sufficient to diagnose an individual, then an internal genital examination using imaging or ultrasounds will be needed for further evaluation.
References
- ↑ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Penile agenesis". www.orpha.net. Retrieved 16 March 2019.
{{cite web}}: CS1 maint: numeric names: authors list (link) - 1 2 "U.K. National Health Service (NHS). 2017-10-18. Retrieved 2024-04-21".
- ↑ "What's wrong with the way intersex has traditionally been treated?". Intersex Society of North America .
- ↑ Meyer-Bahlburg, H.F.L.; Baratz Dalke, K.; Berenbaum, S.A.; Cohen-Kettenis, P.T.; Hines, M.; Schober, J.M. (2016). "Gender Assignment, Reassignment and Outcome in Disorders of Sex Development: Update of the 2005 Consensus Conference". Horm Res Paediatr. 85 (2): 112–118. doi:10.1159/000442386. PMID 26727471. S2CID 32937051.
- ↑ Venkatesh, S. K; Babu, P. R; Joseph, T. P; Varma, K. K (2017). "Male Gender Assignment of a Child with Aphallia and Associated Complex Urological Anomaly". Journal of Indian Association of Pediatric Surgeons. 22 (1): 38–39. doi: 10.4103/0971-9261.194619 . PMC 5217138 . PMID 28082775.
- ↑ Gabler, Tarryn; Charlton, Robyn; Loveland, Jerome; Mapunda, Ellen (2018). "Aphallia: a review to standardize management". Pediatric Surgery International. 34 (8): 813–821. doi:10.1007/s00383-018-4271-z. PMC 5217138 . PMID 28082775. S2CID 4998662.
- ↑ De Castro R, Merlini E, Rigamonti W, Macedo A (2007). "Phalloplasty and urethroplasty in children with penile agenesis: preliminary report". J. Urol. 177 (3): 1112–6, discussion 1117. doi:10.1016/j.juro.2006.10.095. PMID 17296424.
- ↑ Descamps MJ, Hayes PM, Hudson DA (2007). "Phalloplasty in complete aphallia: pedicled anterolateral thigh flap". J Plast Reconstr Aesthet Surg. 62 (3): e51–4. doi:10.1016/j.bjps.2007.04.014. PMID 17574944.
- ↑ Skoog SJ, Belman AB (1989). "Aphallia: its classification and management". J. Urol. 141 (3): 589–92. doi:10.1016/S0022-5347(17)40903-7. PMID 2918598.
- ↑ Chibber PJ, Shah HN, Jain P, Yadav P (2005). "Male gender assignment in aphallia: a case report and review of the literature". Int Urol Nephrol. 37 (2): 317–9. doi:10.1007/s11255-004-7974-0. PMID 16142564. S2CID 30865999.