The gums or gingiva consist of the mucosal tissue that lies over the mandible and maxilla inside the mouth. Gum health and disease can have an effect on general health.
Periodontology or periodontics is the specialty of dentistry that studies supporting structures of teeth, as well as diseases and conditions that affect them. The supporting tissues are known as the periodontium, which includes the gingiva (gums), alveolar bone, cementum, and the periodontal ligament. A periodontist is a dentist that specializes in the prevention, diagnosis and treatment of periodontal disease and in the placement of dental implants.

A periodontal probe is an instrument in dentistry commonly used in the dental armamentarium. It is usually long, thin, and blunted at the end. Its main function is to evaluate the depth of the pockets surrounding a tooth in order to determine the periodontium's overall health. For accuracy and readability, the instrument's head has markings written on it.

Veterinary dentistry is the field of dentistry applied to the care of animals. It is the art and science of prevention, diagnosis, and treatment of conditions, diseases, and disorders of the oral cavity, the maxillofacial region, and its associated structures as it relates to animals.
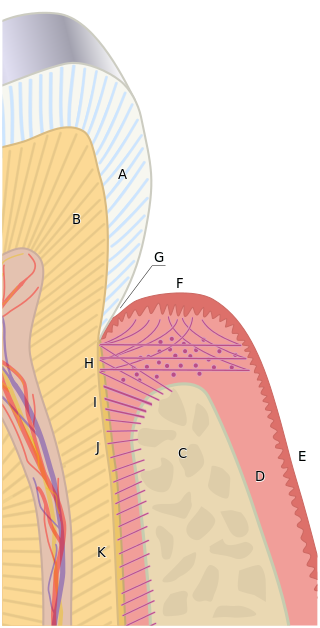
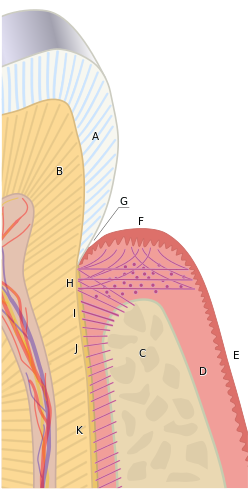
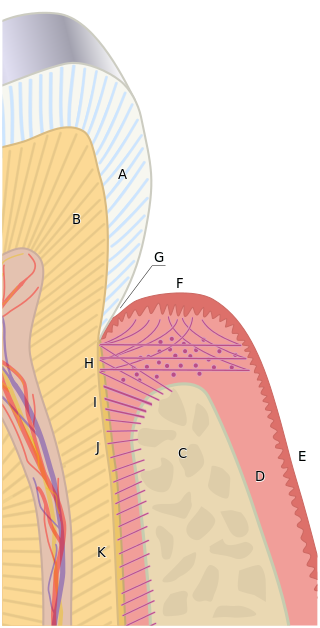
The gingival sulcus is an area of potential space between a tooth and the surrounding gingival tissue and is lined by sulcular epithelium. The depth of the sulcus is bounded by two entities: apically by the gingival fibers of the connective tissue attachment and coronally by the free gingival margin. A healthy sulcular depth is three millimeters or less, which is readily self-cleansable with a properly used toothbrush or the supplemental use of other oral hygiene aids.
Bleeding on probing (BoP) which is also known as bleeding gums or gingival bleeding is a term used by dentists and dental hygienists when referring to bleeding that is induced by gentle manipulation of the tissue at the depth of the gingival sulcus, or interface between the gingiva and a tooth. BoP is a sign of periodontal inflammation and indicates some sort of destruction and erosion to the lining of the sulcus or the ulceration of sulcular epithelium. The blood comes from lamina propria after the ulceration of the lining. BoP seems to be correlated with Periodontal Inflamed Surface Area (PISA).

Scaling and root planing, also known as conventional periodontal therapy, non-surgical periodontal therapy or deep cleaning, is a procedure involving removal of dental plaque and calculus and then smoothing, or planing, of the (exposed) surfaces of the roots, removing cementum or dentine that is impregnated with calculus, toxins, or microorganisms, the agents that cause inflammation. It is a part of non-surgical periodontal therapy. This helps to establish a periodontium that is in remission of periodontal disease. Periodontal scalers and periodontal curettes are some of the tools involved.
The junctional epithelium (JE) is that epithelium which lies at, and in health also defines, the base of the gingival sulcus. The probing depth of the gingival sulcus is measured by a calibrated periodontal probe. In a healthy-case scenario, the probe is gently inserted, slides by the sulcular epithelium (SE), and is stopped by the epithelial attachment (EA). However, the probing depth of the gingival sulcus may be considerably different from the true histological gingival sulcus depth.
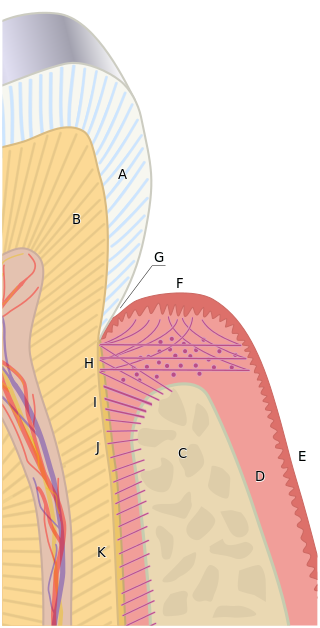
The free gingival margin is the interface between the sulcular epithelium and the epithelium of the oral cavity. This interface exists at the most coronal point of the gingiva, otherwise known as the crest of the marginal gingiva.
A mucogingival junction is an anatomical feature found on the intraoral mucosa. The mucosa of the cheeks and floor of the mouth are freely moveable and fragile, whereas the mucosa around the teeth and on the palate are firm and keratinized. Where the two tissue types meet is known as a mucogingival junction.
The gingival fibers are the connective tissue fibers that inhabit the gingival tissue adjacent to teeth and help hold the tissue firmly against the teeth. They are primarily composed of type I collagen, although type III fibers are also involved.
Gingivectomy is a dental procedure in which a dentist or oral surgeon cuts away part of the gums in the mouth.
Guided bone regeneration (GBR) and guided tissue regeneration (GTR) are dental surgical procedures that use barrier membranes to direct the growth of new bone and gingival tissue at sites with insufficient volumes or dimensions of bone or gingiva for proper function, esthetics or prosthetic restoration. Guided bone regeneration typically refers to ridge augmentation or bone regenerative procedures; guided tissue regeneration typically refers to regeneration of periodontal attachment.

In dentistry, debridement refers to the removal by dental cleaning of accumulations of plaque and calculus (tartar) in order to maintain dental health. Debridement may be performed using ultrasonic instruments, which fracture the calculus, thereby facilitating its removal, as well as hand tools, including periodontal scaler and curettes, or through the use of chemicals such as hydrogen peroxide.

A periodontal abscess, is a localized collection of pus within the tissues of the periodontium. It is a type of dental abscess. A periodontal abscess occurs alongside a tooth, and is different from the more common periapical abscess, which represents the spread of infection from a dead tooth. To reflect this, sometimes the term "lateral (periodontal) abscess" is used. In contrast to a periapical abscess, periodontal abscesses are usually associated with a vital (living) tooth. Abscesses of the periodontium are acute bacterial infections classified primarily by location.
Chronic periodontitis is one of the seven categories of periodontitis as defined by the American Academy of Periodontology 1999 classification system. Chronic periodontitis is a common disease of the oral cavity consisting of chronic inflammation of the periodontal tissues that is caused by the accumulation of profuse amounts of dental plaque. Periodontitis initially begins as gingivitis and can progress onto chronic and subsequent aggressive periodontitis according to the 1999 classification.
In dentistry, numerous types of classification schemes have been developed to describe the teeth and gum tissue in a way that categorizes various defects. All of these classification schemes combine to provide the periodontal diagnosis of the aforementioned tissues in their various states of health and disease.
Clinical attachment loss (CAL) is the predominant clinical manifestation and determinant of periodontal disease.
Periodontal surgery is a form of dental surgery that prevents or corrects anatomical, traumatic, developmental, or plaque-induced defects in the bone, gingiva, or alveolar mucosa. The objectives of this surgery include accessibility of instruments to root surface, elimination of inflammation, creation of an oral environment for plaque control, periodontal diseases control, oral hygiene maintenance, maintain proper embrasure space, address gingiva-alveolar mucosa problems, and esthetic improvement. The surgical procedures include crown lengthening, frenectomy, and mucogingival flap surgery.