Beta cells (β-cells) are specialized endocrine cells located within the pancreatic islets of Langerhans responsible for the production and release of insulin and amylin. Constituting ~50–70% of cells in human islets, beta cells play a vital role in maintaining blood glucose levels. Problems with beta cells can lead to disorders such as diabetes.

Glucagon is a peptide hormone, produced by alpha cells of the pancreas. It raises the concentration of glucose and fatty acids in the bloodstream and is considered to be the main catabolic hormone of the body. It is also used as a medication to treat a number of health conditions. Its effect is opposite to that of insulin, which lowers extracellular glucose. It is produced from proglucagon, encoded by the GCG gene.
Drugs used in diabetes treat diabetes mellitus by decreasing glucose levels in the blood. With the exception of insulin, most GLP-1 receptor agonists, and pramlintide, all diabetes medications are administered orally and are thus called oral hypoglycemic agents or oral antihyperglycemic agents. There are different classes of hypoglycemic drugs, and selection of the appropriate agent depends on the nature of diabetes, age, and situation of the person, as well as other patient factors.

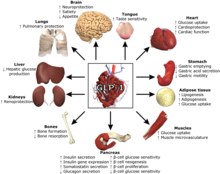
Incretins are a group of metabolic hormones that stimulate a decrease in blood glucose levels. Incretins are released after eating and augment the secretion of insulin released from pancreatic beta cells of the islets of Langerhans by a blood-glucose–dependent mechanism.
Glucose-dependent insulinotropic polypeptide, abbreviated as GIP, is an inhibiting hormone of the secretin family of hormones. While it is a weak inhibitor of gastric acid secretion, its main role, being an incretin, is to stimulate insulin secretion.
Enteroglucagon is a peptide hormone derived from preproglucagon. It is a gastrointestinal hormone, secreted from mucosal cells primarily of the colon and terminal ileum. It consists of 37 amino acids. Enteroglucagon is released when fats and glucose are present in the small intestine; which decrease the motility to allow sufficient time for these nutrients to be absorbed.

Exenatide, sold under the brand name Byetta among others, is a medication used to treat type 2 diabetes. It is used together with diet, exercise, and potentially other antidiabetic medication. It is a treatment option after metformin and sulfonylureas. It is given by injection under the skin.

Vildagliptin, sold under the brand name Galvus and others, is an oral anti-hyperglycemic agent of the dipeptidyl peptidase-4 (DPP-4) inhibitor class of drugs. Vildagliptin inhibits the inactivation of GLP-1 and GIP by DPP-4, allowing GLP-1 and GIP to potentiate the secretion of insulin in the beta cells and suppress glucagon release by the alpha cells of the islets of Langerhans in the pancreas.

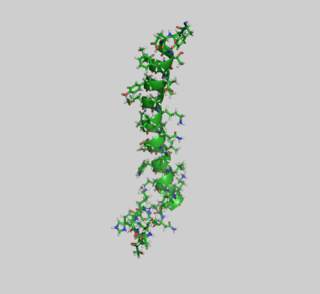
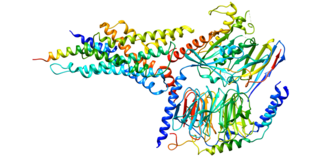
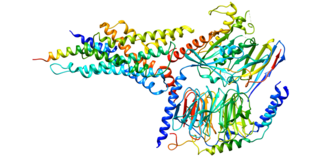
The glucagon-like peptide-1 receptor (GLP1R) is a G protein-coupled receptor (GPCR) found on beta cells of the pancreas and on neurons of the brain. It is involved in the control of blood sugar level by enhancing insulin secretion. In humans it is synthesised by the gene GLP1R, which is present on chromosome 6. It is a member of the glucagon receptor family of GPCRs. GLP1R is composed of two domains, one extracellular (ECD) that binds the C-terminal helix of GLP-1, and one transmembrane (TMD) domain that binds the N-terminal region of GLP-1. In the TMD domain there is a fulcrum of polar residues that regulates the biased signaling of the receptor while the transmembrane helical boundaries and extracellular surface are a trigger for biased agonism.

Structures of GIPR human variant Sun, B., Kobilka, B.K., Sloop, K.W., Feng, D., Kobilka, T.S.
Glucagon-like peptide-2 receptor (GLP-2R) is a protein that in human is encoded by the GLP2R gene located on chromosome 17.

Free fatty acid receptor 2 (FFAR2), also termed G-protein coupled receptor 43 (GPR43), is a rhodopsin-like G-protein coupled receptor. It is coded by the FFAR2 gene. In humans, the FFAR2 gene is located on the long arm of chromosome 19 at position 13.12. Like other GPCRs, FFAR2s reside on the surface membrane of cells and when bond to one of their activating ligands regulate the function of their parent cells. FFAR2 is a member of a small family of structurally and functionally related GPRs termed free fatty acid receptors (FFARs). This family includes three other receptors which, like FFAR2, are activated by certain fatty acids: FFAR1, FFAR3 (GPR41), and FFAR4 (GPR120). FFAR2 and FFAR3 are activated by short-chain fatty acids whereas FFAR1 and FFAR4 are activated by long-chain fatty acids.
Albiglutide is a glucagon-like peptide-1 agonist drug marketed by GlaxoSmithKline (GSK) for treatment of type 2 diabetes. As of 2017 it is unclear if it affects a person's risk of death. GSK has announced that it intends to withdraw the drug from the worldwide market by July 2018 for economic reasons.
Glucagon-like peptide-1 (GLP-1) receptor agonists, also known as GLP-1 analogs, GLP-1DAs or incretin mimetics, are a class of drugs that reduce blood sugar and energy intake by activating the GLP-1 receptor. They mimic the actions of the endogenous incretin hormone GLP-1 that is released by the gut after eating.

Dulaglutide, sold under the brand name Trulicity among others, is a medication used for the treatment of type 2 diabetes in combination with diet and exercise. It is also approved in the United States for the reduction of major adverse cardiovascular events in adults with type 2 diabetes who have established cardiovascular disease or multiple cardiovascular risk factors. It is a once-weekly injection.

Daniel Joshua Drucker is a Canadian endocrinologist. A Fellow of the Royal Society, he is a professor of medicine at the Lunenfeld-Tanenbaum Research Institute, Mount Sinai Hospital, Toronto. He is known for his research into intestinal hormones and their use in the treatment of diabetes, obesity, and other metabolic diseases, as well as intestinal failure.

Omarigliptin (MK-3102) is a potent, long-acting oral antidiabetic drug of the DPP-4 inhibitor class used for once-weekly treatment of type 2 diabetes and currently under development by Merck & Co. It inhibits DPP-4 to increase incretin levels, which inhibit glucagon release, which in turn increases insulin secretion, decreases gastric emptying and decreases blood glucose levels.
Svetlana Mojsov is a Yugoslavian-born chemist who is a research associate professor at Rockefeller University. Her research considers peptide synthesis. She discovered the glucagon-like peptide-1 and uncovered its role in glucose metabolism and the secretion of insulin. Her breakthroughs were transformed by Novo Nordisk into therapeutic agents against diabetes and obesity.
Glucagon receptor agonists are a class of drugs under development for the treatment of obesity, non-alcoholic fatty liver disease, and congenital hyperinsulinism.
GLP1 poly-agonist peptides are a class of drugs that activate multiple peptide hormone receptors including the glucagon-like peptide-1 (GLP-1) receptor. These drugs are developed for the same indications as GLP-1 receptor agonists—especially obesity, type 2 diabetes, and non-alcoholic fatty liver disease. They are expected to provide superior efficacy with fewer adverse effects compared to GLP-1 mono-agonists, which are dose-limited by gastrointestinal disturbances. The effectiveness of multi-receptor agonists could possibly equal or exceed that of bariatric surgery. The first such drug to receive approval is tirzepatide, a dual agonist of GLP-1 and GIP receptors.