Methicillin-resistant Staphylococcus aureus (MRSA) is a group of gram-positive bacteria that are genetically distinct from other strains of Staphylococcus aureus. MRSA is responsible for several difficult-to-treat infections in humans. It caused more than 100,000 deaths worldwide attributable to antimicrobial resistance in 2019.

Klebsiella pneumoniae is a Gram-negative, non-motile, encapsulated, lactose-fermenting, facultative anaerobic, rod-shaped bacterium. It appears as a mucoid lactose fermenter on MacConkey agar.

A hospital-acquired infection, also known as a nosocomial infection, is an infection that is acquired in a hospital or other healthcare facility. To emphasize both hospital and nonhospital settings, it is sometimes instead called a healthcare-associated infection. Such an infection can be acquired in a hospital, nursing home, rehabilitation facility, outpatient clinic, diagnostic laboratory or other clinical settings. A number of dynamic processes can bring contamination into operating rooms and other areas within nosocomial settings. Infection is spread to the susceptible patient in the clinical setting by various means. Healthcare staff also spread infection, in addition to contaminated equipment, bed linens, or air droplets. The infection can originate from the outside environment, another infected patient, staff that may be infected, or in some cases, the source of the infection cannot be determined. In some cases the microorganism originates from the patient's own skin microbiota, becoming opportunistic after surgery or other procedures that compromise the protective skin barrier. Though the patient may have contracted the infection from their own skin, the infection is still considered nosocomial since it develops in the health care setting. Nosocomial infection tends to lack evidence that it was present when the patient entered the healthcare setting, thus meaning it was acquired post-admission.

Vancomycin-resistant Enterococcus, or vancomycin-resistant enterococci (VRE), are bacterial strains of the genus Enterococcus that are resistant to the antibiotic vancomycin.

A needlestick injury is the penetration of the skin by a hypodermic needle or other sharp object that has been in contact with blood, tissue or other body fluids before the exposure. Even though the acute physiological effects of a needlestick injury are generally negligible, these injuries can lead to transmission of blood-borne diseases, placing those exposed at increased risk of infection from disease-causing pathogens, such as the hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV). Among healthcare workers and laboratory personnel worldwide, more than 25 blood-borne virus infections have been reported to have been caused by needlestick injuries. In addition to needlestick injuries, transmission of these viruses can also occur as a result of contamination of the mucous membranes, such as those of the eyes, with blood or body fluids, but needlestick injuries make up more than 80% of all percutaneous exposure incidents in the United States. Various other occupations are also at increased risk of needlestick injury, including law enforcement, laborers, tattoo artists, food preparers, and agricultural workers.
Infection prevention and control is the discipline concerned with preventing healthcare-associated infections; a practical rather than academic sub-discipline of epidemiology. In Northern Europe, infection prevention and control is expanded from healthcare into a component in public health, known as "infection protection". It is an essential part of the infrastructure of health care. Infection control and hospital epidemiology are akin to public health practice, practiced within the confines of a particular health-care delivery system rather than directed at society as a whole.

Taiwan's epidemic of HIV/AIDS began with the first case reported in December 1984. On 17 December 1990 the government promulgated the AIDS Prevention and Control Act. On 11 July 2007, the AIDS Prevention and Control Act was renamed the HIV Infection Control and Patient Rights Protection Act.

The situation with the spread of HIV/AIDS in Russia is described by some researchers as an epidemic. The first cases of human immunodeficiency virus infection were recorded in the USSR in 1985-1987. Patient zero is officially considered to be a military interpreter who worked in Tanzania in the early 1980s and was infected by a local man during sexual contact. After 1988—1989 Elista HIV outbreak, the disease became known to the general public and the first AIDS centers were established. In 1995-1996, the virus spread among injecting drug users (IDUs) and soon expanded throughout the country. By 2006, HIV had spread beyond the vulnerable IDU group, endangering their heterosexual partners and potentially the entire population.

Health in Vietnam encompasses general and specific concerns to the region, its history, and various socioeconomic status, such as dealing with malnutrition, effects of Agent Orange as well as psychological issues from the Vietnam War, tropical diseases, and other issues such as underdeveloped healthcare systems or inadequate ratio of healthcare or social workers to patients.
HIV/AIDS in Eswatini was first reported in 1986 but has since reached epidemic proportions. As of 2016, Eswatini had the highest prevalence of HIV among adults aged 15 to 49 in the world (27.2%).
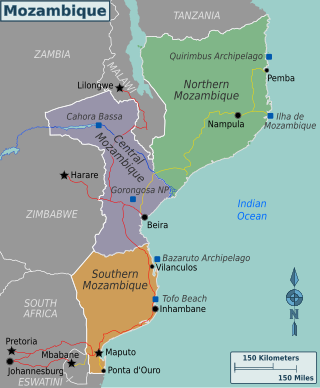
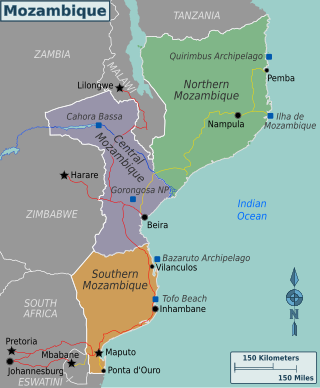
Mozambique is a country particularly hard-hit by the HIV/AIDS epidemic. According to 2008 UNAIDS estimates, this southeast African nation has the 8th highest HIV rate in the world. With 1,600,000 Mozambicans living with HIV, 990,000 of which are women and children, Mozambique's government realizes that much work must be done to eradicate this infectious disease. To reduce HIV/AIDS within the country, Mozambique has partnered with numerous global organizations to provide its citizens with augmented access to antiretroviral therapy and prevention techniques, such as condom use. A surge toward the treatment and prevention of HIV/AIDS in women and children has additionally aided in Mozambique's aim to fulfill its Millennium Development Goals (MDGs). Nevertheless, HIV/AIDS has made a drastic impact on Mozambique; individual risk behaviors are still greatly influenced by social norms, and much still needs to be done to address the epidemic and provide care and treatment to those in need.
With less than 1 percent of the population estimated to be HIV-positive, Egypt is a low-HIV-prevalence country. However, between the years 2006 and 2011, HIV prevalence rates in Egypt increased tenfold. Until 2011, the average number of new cases of HIV in Egypt was 400 per year. But, in 2012 and 2013 it increased to about 600 new cases and in 2014 it reached 880 new cases per year. According to UNAIDS 2016 statistics, there are about 11,000 people currently living with HIV in Egypt. The Ministry of Health and Population reported in 2020 over 13,000 Egyptians are living with HIV/AIDS. However, unsafe behaviors among most-at-risk populations and limited condom usage among the general population place Egypt at risk of a broader epidemic.

Niger is a landlocked country located in West Africa and has Libya, Chad, Nigeria, Benin, Mali, Burkina Faso, and Algeria as its neighboring countries. Niger was French territory that got its independence in 1960 and its official language is French. Niger has an area of 1.267 million square kilometres, nevertheless, 80% of its land area spreads through the Sahara Desert.

Bangladesh is one of the most populous countries in the world, as well as having one of the fastest growing economies in the world. Consequently, Bangladesh faces challenges and opportunities in regards to public health. A remarkable metamorphosis has unfolded in Bangladesh, encompassing the demographic, health, and nutritional dimensions of its populace.

Pneumonia is a common respiratory infection, affecting approximately 450 million people a year and occurring in all parts of the world. It is a major cause of death among all age groups, resulting in 1.4 million deaths in 2010 and 3.0 million deaths in 2016.

Guinea faces a number of ongoing health challenges.

Lesotho's Human development index value for 2018 was 0.518—which put the country in the low human development category—positioning it at 164 out of 189 countries and territories. Health care services in Lesotho are delivered primarily by the government and the Christian Health Association of Lesotho. Access to health services is difficult for many people, especially in rural areas. The country's health system is challenged by the relentless increase of the burden of disease brought about by AIDS, and a lack of expertise and human resources. Serious emergencies are often referred to neighbouring South Africa. The largest contribution to mortality in Lesotho are communicable diseases, maternal, perinatal and nutritional conditions.
Zambia is a landlocked country in Sub Saharan Africa which experiences a burden of both communicable and non-communicable diseases. In line with WHO agenda for equity in health, it has adopted the Universal Health Coverage agenda to mitigate the challenges faced within the health sector. The Ministry of Health (MOH) provides information pertaining to Zambian health. The main focus of the Ministry of Health has been provision of uninterrupted care with emphasis on health systems strengthening and services via the primary health care approach.
Infectious diseases within American correctional settings are a concern within the public health sector. The corrections population is susceptible to infectious diseases through exposure to blood and other bodily fluids, drug injection, poor health care, prison overcrowding, demographics, security issues, lack of community support for rehabilitation programs, and high-risk behaviors. The spread of infectious diseases, such as HIV and other sexually transmitted infections, hepatitis C (HCV), hepatitis B (HBV), and tuberculosis, result largely from needle-sharing, drug use, and consensual and non-consensual sex among prisoners. HIV and hepatitis C need specific attention because of the specific public health concerns and issues they raise.