Related Research Articles

Digitalis is a genus of about 20 species of herbaceous perennial plants, shrubs, and biennials, commonly called foxgloves.

Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia and ventricular fibrillation. When used for local anaesthesia or in nerve blocks, lidocaine typically begins working within several minutes and lasts for half an hour to three hours. Lidocaine mixtures may also be applied directly to the skin or mucous membranes to numb the area. It is often used mixed with a small amount of adrenaline (epinephrine) to prolong its local effects and to decrease bleeding.

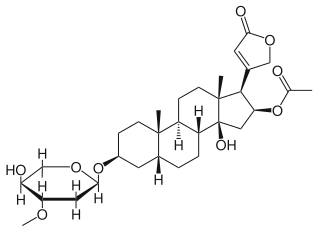
Digoxin, sold under the brand name Lanoxin among others, is a medication used to treat various heart conditions. Most frequently it is used for atrial fibrillation, atrial flutter, and heart failure. Digoxin is one of the oldest medications used in the field of cardiology. It works by increasing myocardial contractility, increasing stroke volume and blood pressure, reducing heart rate, and somewhat extending the time frame of the contraction. Digoxin is taken by mouth or by injection into a vein. Digoxin has a half life of approximately 36 hours given at average doses in patients with normal renal function. It is excreted mostly unchanged in the urine.
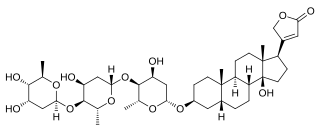
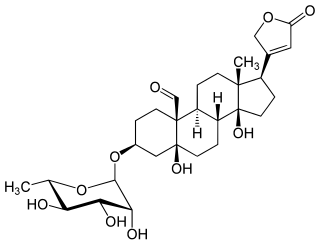
Digitoxin is a cardiac glycoside used for the treatment of heart failure and certain kinds of heart arrhythmia. It is a phytosteroid and is similar in structure and effects to digoxin, though the effects are longer-lasting. Unlike digoxin, which is eliminated from the body via the kidneys, it is eliminated via the liver, and so can be used in patients with poor or erratic kidney function. While several controlled trials have shown digoxin to be effective in a proportion of patients treated for heart failure, the evidence base for digitoxin is not as strong, although it is presumed to be similarly effective.
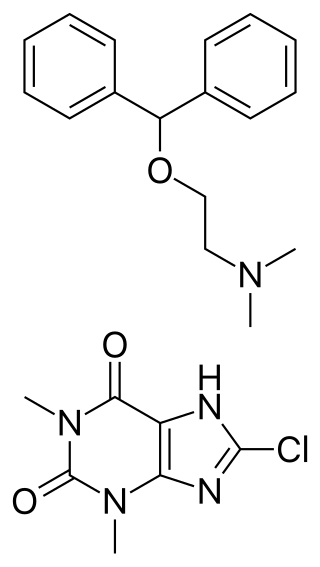
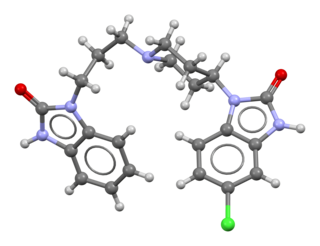
Dimenhydrinate, also known as diphenhydramine/8-chlorotheophylline salt and sold under the brand name Dramamine, among others, is an over-the-counter medication used to treat motion sickness and nausea. Dimenhydrinate is a theoclate salt composed of diphenhydramine and 8-chlorotheophylline in a 1:1 ratio.
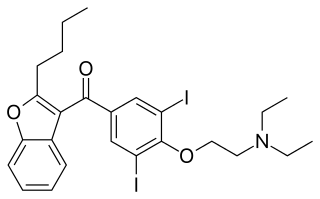
Amiodarone is an antiarrhythmic medication used to treat and prevent a number of types of cardiac dysrhythmias. This includes ventricular tachycardia, ventricular fibrillation, and wide complex tachycardia, atrial fibrillation, and paroxysmal supraventricular tachycardia. Evidence in cardiac arrest, however, is poor. It can be given by mouth, intravenously, or intraosseously. When used by mouth, it can take a few weeks for effects to begin.
Domperidone, sold under the brand name Motilium among others, is a dopamine antagonist medication which is used to treat nausea and vomiting and certain gastrointestinal problems like gastroparesis. It raises the level of prolactin in the human body and is used off label to induce and promote breast milk production. It may be taken by mouth or rectally.

An adverse drug reaction (ADR) is a harmful, unintended result caused by taking medication. ADRs may occur following a single dose or prolonged administration of a drug or may result from the combination of two or more drugs. The meaning of this term differs from the term "side effect" because side effects can be beneficial as well as detrimental. The study of ADRs is the concern of the field known as pharmacovigilance. An adverse event (AE) refers to any unexpected and inappropriate occurrence at the time a drug is used, whether or not the event is associated with the administration of the drug. An ADR is a special type of AE in which a causative relationship can be shown. ADRs are only one type of medication-related harm. Another type of medication-related harm type includes not taking prescribed medications, known as non-adherence. Non-adherence to medications can lead to death and other negative outcomes. Adverse drug reactions require the use of a medication.
Diphenoxylate/atropine, also known as co-phenotrope, is a combination of the medications diphenoxylate and atropine, used to treat diarrhea. It should not be used in those in whom Clostridioides difficile infection is a concern. It is taken by mouth. Onset is typically within an hour.
Prochlorperazine, formerly sold under the brand name Compazine among others, is a medication used to treat nausea, migraines, schizophrenia, psychosis and anxiety. It is a less preferred medication for anxiety. It may be taken by mouth, rectally, injection into a vein, or injection into a muscle.
Benzonatate, sold under the brand name Tessalon among others, is a medication that is used for the symptomatic relief of cough. A 2023 systematic review found that there is inadequate evidence to support the effectiveness and safety of benzonatate for cough and highlighted rising safety concerns. Benzonatate is taken by mouth. Effects generally begin within 20 minutes and last 3 to 8 hours.

Hydroxychloroquine, sold under the brand name Plaquenil among others, is a medication used to prevent and treat malaria in areas where malaria remains sensitive to chloroquine. Other uses include treatment of rheumatoid arthritis, lupus, and porphyria cutanea tarda. It is taken by mouth, often in the form of hydroxychloroquine sulfate.
Voriconazole, sold under the brand name Vfend among others, is an antifungal medication used to treat a number of fungal infections. This includes aspergillosis, candidiasis, coccidioidomycosis, histoplasmosis, penicilliosis, and infections by Scedosporium or Fusarium. It can be taken by mouth or used by injection into a vein.

Digoxin immune fab or digoxin-specific antibody is an antidote for overdose of digoxin. It is made from immunoglobulin fragments from sheep that have already been immunized with a digoxin derivative, digoxindicarboxymethoxylamine (DDMA). Its brand names include Digibind (GlaxoSmithKline) and DigiFab.
Oleandrin is a cardiac glycoside found in the poisonous plant oleander. As a main phytochemical of oleander, oleandrin is associated with the toxicity of oleander sap, and has similar properties to digoxin.

Tricyclic antidepressant overdose is poisoning caused by excessive medication of the tricyclic antidepressant (TCA) type. Symptoms may include elevated body temperature, blurred vision, dilated pupils, sleepiness, confusion, seizures, rapid heart rate, and cardiac arrest. If symptoms have not occurred within six hours of exposure they are unlikely to occur.

Digoxin toxicity, also known as digoxin poisoning, is a type of poisoning that occurs in people who take too much of the medication digoxin or eat plants such as foxglove that contain a similar substance. Symptoms are typically vague. They may include vomiting, loss of appetite, confusion, blurred vision, changes in color perception, and decreased energy. Potential complications include an irregular heartbeat, which can be either too fast or too slow.
Convallatoxin is a glycoside extracted from Convallaria majalis.

Calcium channel blocker toxicity is the taking of too much of the medications known as calcium channel blockers (CCBs), either by accident or on purpose. This often causes a slow heart rate and low blood pressure. This can progress to the heart stopping altogether. Some CCBs can also cause a fast heart rate as a result of the low blood pressure. Other symptoms may include nausea, vomiting, sleepiness, and shortness of breath. Symptoms usually occur in the first six hours but with some forms of the medication may not start until 24 after hours.
The side effects of penicillin are bodily responses to penicillin and closely related antibiotics that do not relate directly to its effect on bacteria. A side effect is an effect that is not intended with normal dosing. Some of these reactions are visible and some occur in the body's organs or blood. Penicillins are a widely used group of medications that are effective for the treatment of a wide variety of bacterial infections in human adults and children as well as other species. Some side effects are predictable, of which some are common but not serious, some are uncommon and serious and others are rare. The route of administration of penicillin can have an effect on the development of side effects. An example of this is irritation and inflammation that develops at a peripheral infusion site when penicillin is administered intravenously. In addition, penicillin is available in different forms. There are different penicillin medications as well as a number of β-lactam antibiotics derived from penicillin.
References
- ↑ Vallerand 2017, pp. 3–4.
- 1 2 3 4 Karch 2017, p. 760.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Vallerand 2017, pp. 424–27.
- ↑ Henry 2016, p. 116.
- ↑ Karch 2017, p. 756.
- ↑ Karch 2017, p. 757.
- ↑ Flanagan RJ, Jones AL (2004). "Fab Antibody Fragments: Some Applications in Clinical Toxicology". Drug Safety. 27 (14): 1115–1133. doi:10.2165/00002018-200427140-00004. PMID 15554746. S2CID 40869324. Archived from the original on 2013-01-16.
- ↑ Vallerand 2017, p. 424-27.
- ↑ Tankenow, Roberta; Tamer, Helen R.; Streetman, Daniel S.; Smith, Scott G.; Welton, Janice L.; Annesley, Thomas; Aaronson, Keith D.; Bleske, Barry E. Interaction Study between Digoxin and a Preparation of Hawthorn (Crataegus oxyacantha), J Clin Pharmacol 2003;43:637-642, accessed May 17, 2017.
- ↑ Goldfrank LW (2006). Goldfrank's Toxicologic Emergencies (8th ed.). New York: McGraw-Hill.