The adenosine A1 receptor (A1AR) [5] is one member of the adenosine receptor group of G protein-coupled receptors with adenosine as endogenous ligand.
The adenosine A1 receptor (A1AR) [5] is one member of the adenosine receptor group of G protein-coupled receptors with adenosine as endogenous ligand.
A1 receptors are implicated in sleep promotion by inhibiting wake-promoting cholinergic neurons in the basal forebrain. [6] A1 receptors are also present in smooth muscle throughout the vascular system. [7]
The adenosine A1 receptor has been found to be ubiquitous throughout the entire body.[ citation needed ]
Activation of the adenosine A1 receptor by an agonist causes binding of Gi1/2/3 or Go protein. Binding of Gi1/2/3 causes an inhibition of adenylate cyclase and, therefore, a decrease in the cAMP concentration. An increase of the inositol triphosphate/diacylglycerol concentration is caused by an activation of phospholipase C, whereas the elevated levels of arachidonic acid are mediated by DAG lipase, which cleaves DAG to form arachidonic acid. Several types of potassium channels are activated but N-, P-, and Q-type calcium channels are inhibited. [8]
This receptor has an inhibitory function on most of the tissues in which it rests. In the brain, it slows metabolic activity by a combination of actions. At the neuron's synapse, it reduces synaptic vesicle release.[ citation needed ]
Caffeine, as well as theophylline, has been found to antagonize both A1 and A2A receptors in the brain.[ citation needed ]
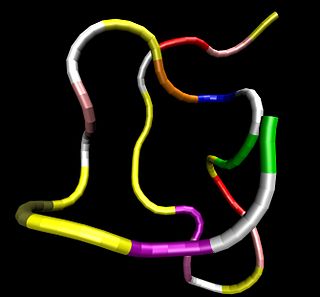
((R)-tetrahydrofuran-3-ylamino)-9H-purin-9-yl)-tetrashydrofuran3,4-diol) [9]
In the heart, A1 receptors play roles in electrical pacing (chronotropy and dromotropy), fluid balance, local sympathetic regulation, and metabolism. [9]
When bound by adenosine, A1 receptors inhibit impulses generated in supraventricular tissue (SA node, AV node) and the Bundle of His/Purkinje system, leading to negative chronotropy (slowing of the heart rate). [9] Specifically, A1 receptor activation leads to inactivation of the inwardly rectifying K+ current and inhibition of the inward Ca2+ current (ICa) and the 'funny' hyperpolarization-activated current (If). [17] Adenosine agonism of A1ARs also inhibits release of norepinephrine from cardiac nerves. [18] Norepinephrine is a positive chronotrope, inotrope, and dromotrope, through its agonism of β adrenergic receptors on pacemaker cells and ventricular myocytes. [19] [20]
Collectively, these mechanisms lead to an myocardial depressant effect by decreasing the conduction of electrical impulses and suppressing pacemaker cells function, resulting in a decrease in heart rate. This makes adenosine a useful medication for treating and diagnosing tachyarrhythmias, or excessively fast heart rates. This effect on the A1 receptor also explains why there is a brief moment of cardiac standstill when adenosine is administered as a rapid IV push during cardiac resuscitation.[ citation needed ] The rapid infusion causes a momentary myocardial stunning effect.
In normal physiological states, this serves as protective mechanisms. However, in altered cardiac function, such as hypoperfusion caused by hypotension, heart attack or cardiac arrest caused by nonperfusing bradycardias, adenosine has a negative effect on physiological functioning by preventing necessary compensatory increases in heart rate and blood pressure that attempt to maintain cerebral perfusion.[ citation needed ]
Metabolically, A1AR activation by endogenous adenosine across the body reduces plasma glucose, lactate, and insulin levels, however A2aR activation increased glucose and lactate levels to an extent greater than the A1AR effect on glucose and lactate. [21] Thus, intravascular administration of adenosine increases the amount of glucose and lactate available in the blood for cardiac myocytes. A1AR activation also partially inhibits glycolysis, slowing its rate to align with oxidative metabolism, which limits post-ischemic damage through reduced H+ generation. [22]
In the state of myocardial hypertrophy and remodeling, interstitial adenosine and the expression of the A1AR receptor are both increased. After transition to heart failure however, overexpression of A1AR is no longer present. [23] Excess A1AR expression can induce cardiomyopathy, cardiac dilatation, and cardiac hypertrophy. [24] Cardiac failure may involve increased A1AR expression and decreased adenosine in physical models of cardiac overload and in dysfunction induced by TNFα. [25] Heart failure often involves secretion of atrial natriuretic peptide to compensate for reduced renal perfusion and thus, secretion of electrolytes. A1AR activation also increases secretion of atrial natriuretic peptide from atrial myocytes. [26] [27]

Adenosine (symbol A) is an organic compound that occurs widely in nature in the form of diverse derivatives. The molecule consists of an adenine attached to a ribose via a β-N9-glycosidic bond. Adenosine is one of the four nucleoside building blocks of RNA (and its derivative deoxyadenosine is a building block of DNA), which are essential for all life on earth. Its derivatives include the energy carriers adenosine mono-, di-, and triphosphate, also known as AMP/ADP/ATP. Cyclic adenosine monophosphate (cAMP) is pervasive in signal transduction. Adenosine is used as an intravenous medication for some cardiac arrhythmias.
An antiplatelet drug (antiaggregant), also known as a platelet agglutination inhibitor or platelet aggregation inhibitor, is a member of a class of pharmaceuticals that decrease platelet aggregation and inhibit thrombus formation. They are effective in the arterial circulation where classical Vitamin K antagonist anticoagulants have minimal effect.

Beta blockers, also spelled β-blockers, are a class of medications that are predominantly used to manage abnormal heart rhythms (arrhythmia), and to protect the heart from a second heart attack after a first heart attack. They are also widely used to treat high blood pressure, although they are no longer the first choice for initial treatment of most patients.

Angiotensin is a peptide hormone that causes vasoconstriction and an increase in blood pressure. It is part of the renin–angiotensin system, which regulates blood pressure. Angiotensin also stimulates the release of aldosterone from the adrenal cortex to promote sodium retention by the kidneys.
Atrial natriuretic peptide (ANP) or atrial natriuretic factor (ANF) is a natriuretic peptide hormone secreted from the cardiac atria that in humans is encoded by the NPPA gene. Natriuretic peptides are a family of hormone/paracrine factors that are structurally related. The main function of ANP is causing a reduction in expanded extracellular fluid (ECF) volume by increasing renal sodium excretion. ANP is synthesized and secreted by cardiac muscle cells in the walls of the atria in the heart. These cells contain volume receptors which respond to increased stretching of the atrial wall due to increased atrial blood volume.

Vasodilation, also known as vasorelaxation, is the widening of blood vessels. It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins, large arteries, and smaller arterioles. The process is the opposite of vasoconstriction, which is the narrowing of blood vessels.

The adenosine receptors (or P1 receptors) are a class of purinergic G protein-coupled receptors with adenosine as the endogenous ligand. There are four known types of adenosine receptors in humans: A1, A2A, A2B and A3; each is encoded by a different gene.

The baroreflex or baroreceptor reflex is one of the body's homeostatic mechanisms that helps to maintain blood pressure at nearly constant levels. The baroreflex provides a rapid negative feedback loop in which an elevated blood pressure causes the heart rate to decrease. Decreased blood pressure decreases baroreflex activation and causes heart rate to increase and to restore blood pressure levels. Their function is to sense pressure changes by responding to change in the tension of the arterial wall The baroreflex can begin to act in less than the duration of a cardiac cycle and thus baroreflex adjustments are key factors in dealing with postural hypotension, the tendency for blood pressure to decrease on standing due to gravity.
In cardiology, ventricular remodeling refers to changes in the size, shape, structure, and function of the heart. This can happen as a result of exercise or after injury to the heart muscle. The injury is typically due to acute myocardial infarction, but may be from a number of causes that result in increased pressure or volume, causing pressure overload or volume overload on the heart. Chronic hypertension, congenital heart disease with intracardiac shunting, and valvular heart disease may also lead to remodeling. After the insult occurs, a series of histopathological and structural changes occur in the left ventricular myocardium that lead to progressive decline in left ventricular performance. Ultimately, ventricular remodeling may result in diminished contractile (systolic) function and reduced stroke volume.

T-tubules are extensions of the cell membrane that penetrate into the center of skeletal and cardiac muscle cells. With membranes that contain large concentrations of ion channels, transporters, and pumps, T-tubules permit rapid transmission of the action potential into the cell, and also play an important role in regulating cellular calcium concentration.

The beta-1 adrenergic receptor, also known as ADRB1, can refer to either the protein-encoding gene or one of the four adrenergic receptors. It is a G-protein coupled receptor associated with the Gs heterotrimeric G-protein that is expressed predominantly in cardiac tissue. In addition to cardiac tissue, beta-1 adrenergic receptors are also expressed in the cerebral cortex.

Norepinephrine (NE), also called noradrenaline (NA) or noradrenalin, is an organic chemical in the catecholamine family that functions in the brain and body as both a hormone and neurotransmitter. The name "noradrenaline" is more commonly used in the United Kingdom, whereas "norepinephrine" is usually preferred in the United States. "Norepinephrine" is also the international nonproprietary name given to the drug. Regardless of which name is used for the substance itself, parts of the body that produce or are affected by it are referred to as noradrenergic.
Bathmotropic often refers to modifying the degree of excitability specifically of the heart; in general, it refers to modification of the degree of excitability of musculature in general, including the heart. It especially is used to describe the effects of the cardiac nerves on cardiac excitability. Positive bathmotropic effects increase the response of muscle to stimulation, whereas negative bathmotropic effects decrease the response of muscle to stimulation. In a whole, it is the heart's reaction to catecholamines. Conditions that decrease bathmotropy cause the heart to be less responsive to catecholaminergic drugs. A substance that has a bathmotropic effect is known as a bathmotrope.
Cardiorenal syndrome (CRS) is an umbrella term used in the medical field that defines disorders of the heart and kidneys whereby "acute or chronic dysfunction in one organ may induce acute or chronic dysfunction of the other". When one of these organs fails, the other may subsequently fail. The heart and the kidneys are involved in maintaining hemodynamic stability and organ perfusion through an intricate network. Patients who have renal failure first may be hard to determine if heart failure is concurrent. These two organs communicate with one another through a variety of pathways in an interdependent relationship. In a 2004 report from the National Heart, Lung and Blood Institute, CRS was defined as a condition where treatment of congestive heart failure is limited by decline in kidney function. This definition has since been challenged repeatedly but there still remains little consensus over a universally accepted definition for CRS. At a consensus conference of the Acute Dialysis Quality Initiative (ADQI), the CRS was classified into five subtypes primarily based upon the organ that initiated the insult as well as the acuity of disease.

Cardiac magnetic resonance imaging perfusion, also known as stress CMR perfusion, is a clinical magnetic resonance imaging test performed on patients with known or suspected coronary artery disease to determine if there are perfusion defects in the myocardium of the left ventricle that are caused by narrowing of one or more of the coronary arteries.
Cenderitide is a natriuretic peptide developed by the Mayo Clinic as a potential treatment for heart failure. Cenderitide is created by the fusion of the 15 amino acid C-terminus of the snake venom dendroaspis natriuretic peptide (DNP) with the full C-type natriuretic peptide (CNP) structure. This peptide chimera is a dual activator of the natriuretic peptide receptors NPR-A and NPR-B and therefore exhibits the natriuretic and diuretic properties of DNP, as well as the antiproliferative and antifibrotic properties of CNP.
Serelaxin is a medication which is marketed in Russia for the treatment of acute heart failure (AHF), targeting the relaxin receptor. It was also under development in other places in the world, including in the United States, Europe, and Asia, but ultimately was not marketed in these areas.

Purinergic signalling is a form of extracellular signalling mediated by purine nucleotides and nucleosides such as adenosine and ATP. It involves the activation of purinergic receptors in the cell and/or in nearby cells, thereby regulating cellular functions.
Cardioprotection includes all mechanisms and means that contribute to the preservation of the heart by reducing or even preventing myocardial damage. Cardioprotection encompasses several regimens that have shown to preserve function and viability of cardiac muscle cell tissue subjected to ischemic insult or reoxygenation. Cardioprotection includes strategies that are implemented before an ischemic event, during an ischemic event and after the event and during reperfusion. These strategies can be further stratified by performing the intervention locally or remotely, creating classes of conditioning known as remote ischemic PC (RIPC), remote ischemic PostC and remote ischemic PerC. Classical (local) preconditioning has an early phase with an immediate onset lasting 2–3 hours that protects against myocardial infarction. The early phase involves post-translational modification of preexisting proteins, brought about by the activation of G protein-coupled receptors as well as downstream MAPK's and PI3/Akt. These signaling events act on the ROS-generating mitochondria, activate PKCε and the Reperfusion Injury Salvage Kinase (RISK) pathway, preventing mitochondrial permeability transition pore (MTP) opening. The late phase with an onset of 12–24 hours that lasts 3–4 days and protects against both infarction and reversible postischemic contractile dysfunction, termed myocardial stunning. This phase involves the synthesis of new cardioprotective proteins stimulated by nitric oxide (NO), ROS and adenosine acting on kinases such as PKCε and Src, which in turn activate gene transcription and upregulation of late PC molecular players.

Brain natriuretic peptide 32 (BNP), also known as B-type natriuretic peptide, is a hormone secreted by cardiomyocytes in the heart ventricles in response to stretching caused by increased ventricular blood volume. Along with NT-proBNP, BNP is one of two natriuretic peptides.