Mastectomy is the medical term for the surgical removal of one or both breasts, partially or completely. A mastectomy is usually carried out to treat breast cancer. In some cases, women believed to be at high risk of breast cancer have the operation as a preventive measure. Alternatively, some women can choose to have a wide local excision, also known as a lumpectomy, an operation in which a small volume of breast tissue containing the tumor and a surrounding margin of healthy tissue is removed to conserve the breast. Both mastectomy and lumpectomy are referred to as "local therapies" for breast cancer, targeting the area of the tumor, as opposed to systemic therapies, such as chemotherapy, hormonal therapy, or immunotherapy.

Thyroid neoplasm is a neoplasm or tumor of the thyroid. It can be a benign tumor such as thyroid adenoma, or it can be a malignant neoplasm, such as papillary, follicular, medullary or anaplastic thyroid cancer. Most patients are 25 to 65 years of age when first diagnosed; women are more affected than men. The estimated number of new cases of thyroid cancer in the United States in 2010 is 44,670 compared to only 1,690 deaths. Of all thyroid nodules discovered, only about 5 percent are cancerous, and under 3 percent of those result in fatalities.

Multiple endocrine neoplasia is a condition which encompasses several distinct syndromes featuring tumors of endocrine glands, each with its own characteristic pattern. In some cases, the tumors are malignant, in others, benign. Benign or malignant tumors of nonendocrine tissues occur as components of some of these tumor syndromes.

Calcitonin is a 32 amino acid peptide hormone secreted by parafollicular cells (also known as C cells) of the thyroid (or endostyle) in humans and other chordates in the ultimopharyngeal body. It acts to reduce blood calcium (Ca2+), opposing the effects of parathyroid hormone (PTH).
Adrenocortical carcinoma (ACC) is an aggressive cancer originating in the cortex of the adrenal gland.
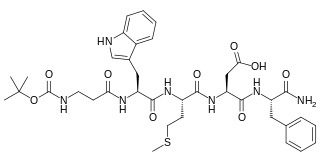
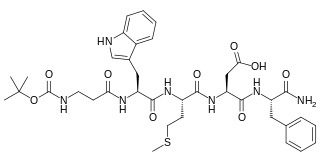
Pentagastrin is a synthetic polypeptide that has effects like gastrin when given parenterally. It stimulates the secretion of gastric acid, pepsin, and intrinsic factor, and has been used as a diagnostic aid as the pentagastrin-stimulated calcitonin test.
This is a list of terms related to oncology. The original source for this list was the US National Cancer Institute's public domain Dictionary of Cancer Terms.

Multiple endocrine neoplasia type 2 is a group of medical disorders associated with tumors of the endocrine system. The tumors may be benign or malignant (cancer). They generally occur in endocrine organs, but may also occur in endocrine tissues of organs not classically thought of as endocrine. MEN2 is a sub-type of MEN and itself has sub-types, as discussed below. Variants in MEN2A have been associated with Hirschsprung disease. Screening for this condition can begin as young as eight years old for Pheochromocytoma.

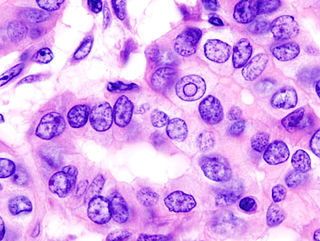
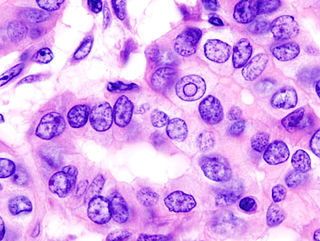
A Hürthle cell is a cell in the thyroid that is often associated with Hashimoto's thyroiditis as well as benign and malignant tumors. This version is a relatively rare form of differentiated thyroid cancer, accounting for only 3-10% of all differentiated thyroid cancers. Oncocytes in the thyroid are often called Hürthle cells. Although the terms oncocyte, oxyphilic cell, and Hürthle cell are used interchangeably, Hürthle cell is used only to indicate cells of thyroid follicular origin.

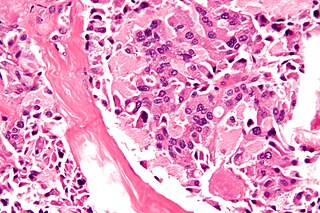
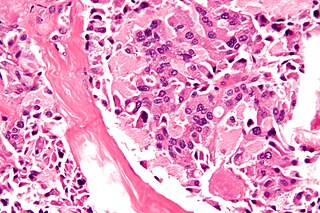
Anaplastic thyroid cancer (ATC), also known as anaplastic thyroid carcinoma, is an aggressive form of thyroid cancer characterized by uncontrolled growth of cells in the thyroid gland. This form of cancer generally carries a very poor prognosis due to its aggressive behavior and resistance to cancer treatments. The cells of anaplastic thyroid cancer are highly abnormal and usually no longer resemble the original thyroid cells and have poor differentiation.

Papillary thyroid cancer is the most common type of thyroid cancer, representing 75 percent to 85 percent of all thyroid cancer cases. It occurs more frequently in women and presents in the 20–55 year age group. It is also the predominant cancer type in children with thyroid cancer, and in patients with thyroid cancer who have had previous radiation to the head and neck. It is often well-differentiated, slow-growing, and localized, although it can metastasize.

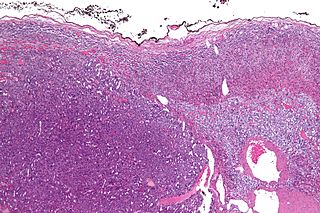
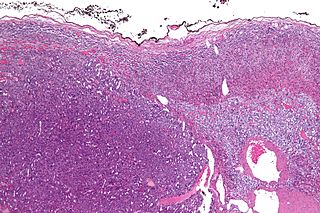
Nasopharyngeal carcinoma (NPC), or nasopharynx cancer, is the most common cancer originating in the nasopharynx, most commonly in the postero-lateral nasopharynx or pharyngeal recess, accounting for 50% of cases. NPC occurs in children and adults. NPC differs significantly from other cancers of the head and neck in its occurrence, causes, clinical behavior, and treatment. It is vastly more common in certain regions of East Asia and Africa than elsewhere, with viral, dietary and genetic factors implicated in its causation. It is most common in males. It is a squamous cell carcinoma of an undifferentiated type. Squamous epithelial cells are a flat type of cell found in the skin and the membranes that line some body cavities. Undifferentiated cells are cells that do not have their mature features or functions.

The RETproto-oncogene encodes a receptor tyrosine kinase for members of the glial cell line-derived neurotrophic factor (GDNF) family of extracellular signalling molecules. RET loss of function mutations are associated with the development of Hirschsprung's disease, while gain of function mutations are associated with the development of various types of human cancer, including medullary thyroid carcinoma, multiple endocrine neoplasias type 2A and 2B, pheochromocytoma and parathyroid hyperplasia.
Multiple endocrine neoplasia type 2B is a genetic disease that causes multiple tumors on the mouth, eyes, and endocrine glands. It is the most severe type of multiple endocrine neoplasia, differentiated by the presence of benign oral and submucosal tumors in addition to endocrine malignancies. It was first described by Wagenmann in 1922, and was first recognized as a syndrome in 1965-1966 by E.D. Williams and D.J. Pollock. It is caused by the pathogenic variant p.Met918Thr in the RET gene. This variant can cause medullary thyroid cancer and Pheochromocytoma. Presentation can include a Marfanoid body, enlarged lips, and ganglionueuromas.

Parathyroid carcinoma is a rare cancer resulting in parathyroid adenoma to carcinoma progression. It forms in tissues of one or more of the parathyroid glands.

Male breast cancer (MBC) is a cancer in males that originates in their breasts. Males account for less than 1% of new breast cancers with about 20,000 new cases being diagnosed worldwide every year. Its incidence rates in males vs. females are, respectively, 0.4 and 66.7 per 100,000 person-years. The worldwide incidences of male as well as female breast cancers have been increasing over the last few decades. Currently, one of every 800 men are estimated to develop this cancer during their lifetimes.
Renal medullary carcinoma is a rare type of cancer that affects the kidney. It tends to be aggressive, difficult to treat, and is often metastatic at the time of diagnosis. Most individuals with this type of cancer have sickle cell trait or rarely sickle cell disease, suggesting that the sickle cell trait may be a risk factor for this type of cancer.
Thyroid cancer is cancer that develops from the tissues of the thyroid gland. It is a disease in which cells grow abnormally and have the potential to spread to other parts of the body. Symptoms can include swelling or a lump in the neck. Cancer can also occur in the thyroid after spread from other locations, in which case it is not classified as thyroid cancer.

Selpercatinib, sold under the brand name Retevmo among others, is a medication for the treatment of cancers in people whose tumors have an alteration in a specific gene. It is taken by mouth.
Mammary secretory carcinoma (MSC), also termed secretory carcinoma of the breast, is a rare form of the breast cancers. MSC usually affects women but in a significant percentage of cases also occurs in men and children. Indeed, McDvitt and Stewart first described MSC in 1966 and termed it juvenile breast carcinoma because an increased number of cases were at that time diagnosed in juvenile females. MSC is the most common form of breast cancer in children, representing 80% of childhood breast cancers, although it accounts for less than 0.15% of all breast cancers.