Related Research Articles

Hypoglycemia, also called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose below 70 mg/dL (3.9 mmol/L), symptoms associated with hypoglycemia, and resolution of symptoms when blood sugar returns to normal. Hypoglycemia may result in headache, tiredness, clumsiness, trouble talking, confusion, fast heart rate, sweating, shakiness, nervousness, hunger, loss of consciousness, seizures, or death. Symptoms typically come on quickly.

A brain tumor occurs when abnormal cells form within the brain. There are two main types of tumors: malignant tumors and benign (non-cancerous) tumors. These can be further classified as primary tumors, which start within the brain, and secondary tumors, which most commonly have spread from tumors located outside the brain, known as brain metastasis tumors. All types of brain tumors may produce symptoms that vary depending on the size of the tumor and the part of the brain that is involved. Where symptoms exist, they may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking, with sensations, or unconsciousness.

Metastasis is a pathogenic agent's spread from an initial or primary site to a different or secondary site within the host's body; the term is typically used when referring to metastasis by a cancerous tumor. The newly pathological sites, then, are metastases (mets). It is generally distinguished from cancer invasion, which is the direct extension and penetration by cancer cells into neighboring tissues.

A bone tumor is an abnormal growth of tissue in bone, traditionally classified as noncancerous (benign) or cancerous (malignant). Cancerous bone tumors usually originate from a cancer in another part of the body such as from lung, breast, thyroid, kidney and prostate. There may be a lump, pain, or neurological signs from pressure. A bone tumor might present with a pathologic fracture. Other symptoms may include fatigue, fever, weight loss, anemia and nausea. Sometimes there are no symptoms and the tumour is found when investigating another problem.

An insulinoma is a tumour of the pancreas that is derived from beta cells and secretes insulin. It is a rare form of a neuroendocrine tumour. Most insulinomas are benign in that they grow exclusively at their origin within the pancreas, but a minority metastasize. Insulinomas are one of the functional pancreatic neuroendocrine tumour (PNET) group. In the Medical Subject Headings classification, insulinoma is the only subtype of "islet cell adenoma".
Hyperinsulinemic hypoglycemia describes the condition and effects of low blood glucose caused by excessive insulin. Hypoglycemia due to excess insulin is the most common type of serious hypoglycemia. It can be due to endogenous or injected insulin.
Hyperinsulinism refers to an above normal level of insulin in the blood of a person or animal. Normal insulin secretion and blood levels are closely related to the level of glucose in the blood, so that a given level of insulin can be normal for one blood glucose level but low or high for another. Hyperinsulinism can be associated with several types of medical problems, which can be roughly divided into two broad and largely non-overlapping categories: those tending toward reduced sensitivity to insulin and high blood glucose levels (hyperglycemia), and those tending toward excessive insulin secretion and low glucose levels (hypoglycemia).
Whipple's triad is a collection of three signs that suggests that a patient's symptoms result from hypoglycaemia that may indicate insulinoma. The essential conditions are symptoms of hypoglycaemia, low blood plasma glucose concentration, and relief of symptoms when plasma glucose concentration is increased. It was first described by the pancreatic surgeon Allen Whipple, who aimed to establish criteria for exploratory pancreatic surgery to look for insulinoma.

Congenital hyperinsulinism (HI or CHI) is a rare condition causing severe hypoglycemia in newborns due to the overproduction of insulin. There are various causes of HI, some of which are known to be the result of a genetic mutation. Sometimes HI occurs on its own (isolated) and more rarely associated with other medical conditions.

A benign tumor is a mass of cells (tumor) that does not invade neighboring tissue or metastasize. Compared to malignant (cancerous) tumors, benign tumors generally have a slower growth rate. Benign tumors have relatively well differentiated cells. They are often surrounded by an outer surface or stay contained within the epithelium. Common examples of benign tumors include moles and uterine fibroids.

Diazoxide, sold under the brand name Proglycem and others, is a medication used to treat low blood sugar due to a number of specific causes. This includes islet cell tumors that cannot be removed and leucine sensitivity. It can also be used in refractory cases of sulfonylurea toxicity. It is generally taken by mouth.

Diabetic hypoglycemia is a low blood glucose level occurring in a person with diabetes mellitus. It is one of the most common types of hypoglycemia seen in emergency departments and hospitals. According to the National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP), and based on a sample examined between 2004 and 2005, an estimated 55,819 cases involved insulin, and severe hypoglycemia is likely the single most common event.

Multiple endocrine neoplasia type 1 (MEN-1) is one of a group of disorders, the multiple endocrine neoplasias, that affect the endocrine system through development of neoplastic lesions in pituitary, parathyroid gland and pancreas. Individuals suffering from this disorder are prone to developing multiple endocrine and nonendocrine tumors. It was first described by Paul Wermer in 1954.
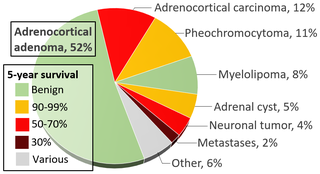
An adrenal tumor or adrenal mass is any benign or malignant neoplasms of the adrenal gland, several of which are notable for their tendency to overproduce endocrine hormones. Adrenal cancer is the presence of malignant adrenal tumors, and includes neuroblastoma, adrenocortical carcinoma and some adrenal pheochromocytomas. Most adrenal pheochromocytomas and all adrenocortical adenomas are benign tumors, which do not metastasize or invade nearby tissues, but may cause significant health problems by unbalancing hormones.

Acromegaly is a disorder that results in excess growth of certain parts of the human body. It is caused by excess growth hormone (GH) after the growth plates have closed. The initial symptom is typically enlargement of the hands and feet. There may also be an enlargement of the forehead, jaw, and nose. Other symptoms may include joint pain, thicker skin, deepening of the voice, headaches, and problems with vision. Complications of the disease may include type 2 diabetes, sleep apnea, and high blood pressure.
Neuro-oncology is the study of brain and spinal cord neoplasms, many of which are very dangerous and life-threatening. Among the malignant brain cancers, gliomas of the brainstem and pons, glioblastoma multiforme, and high-grade astrocytoma/oligodendroglioma are among the worst. In these cases, untreated survival usually amounts to only a few months, and survival with current radiation and chemotherapy treatments may extend that time from around a year to a year and a half, possibly two or more, depending on the patient's condition, immune function, treatments used, and the specific type of malignant brain neoplasm. Surgery may in some cases be curative, but, as a general rule, malignant brain cancers tend to regenerate and emerge from remission easily, especially highly malignant cases. In such cases, the goal is to excise as much of the mass and as much of the tumor margin as possible without endangering vital functions or other important cognitive abilities. The Journal of Neuro-Oncology is the longest continuously published journal in the field and serves as a leading reference to those practicing in the area of neuro-oncology.

Pancreatic neuroendocrine tumours, often referred to as "islet cell tumours", or "pancreatic endocrine tumours" are neuroendocrine neoplasms that arise from cells of the endocrine (hormonal) and nervous system within the pancreas.
Glucose-elevating agents are medications used to treat hypoglycemia by raising blood glucose. In diabetics, hypoglycemia can occur as a result of too much insulin or antidiabetic medication, insufficient food intake, or sudden increase in physical activity or exercise. The most common glucose-elevating agents used to treat diabetic hypoglycemia are glucose and glucagon injections when severe hypoglycemia occurs. Diazoxide, which is used to counter hypoglycemia in disease states such as insulinoma or congenital hyperinsulinism, increases blood glucose and decreases insulin secretion and glucagon accelerates breakdown of glycogen in the liver (glycogenolysis) to release glucose into the bloodstream.
Ovarian germ cell tumors (OGCTs) are heterogeneous tumors that are derived from the primitive germ cells of the embryonic gonad, which accounts for about 2.6% of all ovarian malignancies. There are four main types of OGCTs, namely dysgerminomas, yolk sac tumor, teratoma, and choriocarcinoma.
References
- ↑ Hagel AF, Hagel WH, Lindner AS, Kammerer FJ, Neurath MF, Konturek PC, Harsch IA (August 2011). "Metastatic insulinoma - prolonged survival after multimodal approach". Medical Science Monitor. 17 (8): CS103-107. doi:10.12659/msm.881891. PMC 3539604 . PMID 21804467.
- ↑ Bernard V, Lombard-Bohas C, Taquet MC, Caroli-Bosc FX, Ruszniewski P, Niccoli P, et al. (May 2013). "Efficacy of everolimus in patients with metastatic insulinoma and refractory hypoglycemia". European Journal of Endocrinology. 168 (5): 665–74. doi: 10.1530/EJE-12-1101 . PMID 23392213.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Yu J, Ping F, Zhang H, Li W, Yuan T, Fu Y, et al. (December 2018). "Clinical Management of Malignant Insulinoma: a single institution's experience over three decades". BMC Endocrine Disorders. 18 (1): 92. doi: 10.1186/s12902-018-0321-8 . PMC 6282250 . PMID 30522468.
- ↑ Meleth S, Whitehead N, Evans TS, Lux L, eds. (February 2013). "Common sites of metastasis for different primary sites". Technology Assessment on Genetic Testing or Molecular Pathology Testing of Cancers with Unknown Primary Site to Determine Origin. Rockville (MD): Agency for Healthcare Research and Quality (US).
- 1 2 3 4 Taye A, Libutti SK (August 2015). "Diagnosis and management of insulinoma: current best practice and ongoing developments". Research and Reports in Endocrine Disorders. 5: 125–33. doi: 10.2147/RRED.S86565 .
- 1 2 de Herder WW, van Schaik E, Kwekkeboom D, Feelders RA (September 2011). "New therapeutic options for metastatic malignant insulinomas". Clinical Endocrinology. 75 (3): 277–84. doi: 10.1111/j.1365-2265.2011.04145.x . PMID 21649688.
- ↑ Miranda G (June 2018). "Malignant insulinoma chemotherapy resistant, pancreatic neuroendocrine tumor of uncertain prognosis". Journal of Clinical and Translational Endocrinology: Case Reports. 8: 16–18. doi: 10.1016/j.jecr.2018.01.001 .
- ↑ Iglesias P, Díez JJ (April 2014). "Management of endocrine disease: a clinical update on tumor-induced hypoglycemia". European Journal of Endocrinology. 170 (4): R147-57. doi: 10.1530/eje-13-1012 . PMID 24459236.