The ovary is a gonad in the female reproductive system that produces ova. When an ovum is released, this travels through the fallopian tube/oviduct into the uterus. There is an ovary found on the left and the right side of the body. The ovaries also secrete hormones that play a role in the menstrual cycle and fertility. The ovary progresses through many stages beginning in the prenatal period through menopause. It is also an endocrine gland because of the various hormones that it secretes.

The menstrual cycle is a series of natural changes in hormone production and the structures of the uterus and ovaries of the female reproductive system that makes pregnancy possible. The ovarian cycle controls the production and release of eggs and the cyclic release of estrogen and progesterone. The uterine cycle governs the preparation and maintenance of the lining of the uterus (womb) to receive an embryo. These cycles are concurrent and coordinated, normally last between 21 and 35 days, with a median length of 28 days, and continue for about 30–45 years.

Ovulation is the release of eggs from the ovaries. In women, this event occurs when the ovarian follicles rupture and release the secondary oocyte ovarian cells. After ovulation, during the luteal phase, the egg will be available to be fertilized by sperm. In addition, the uterine lining (endometrium) is thickened to be able to receive a fertilized egg. If no conception occurs, the uterine lining as well as the egg will be shed during menstruation.
Luteinizing hormone is a hormone produced by gonadotropic cells in the anterior pituitary gland. The production of LH is regulated by gonadotropin-releasing hormone (GnRH) from the hypothalamus. In females, an acute rise of LH known as an LH surge, triggers ovulation and development of the corpus luteum. In males, where LH had also been called interstitial cell–stimulating hormone (ICSH), it stimulates Leydig cell production of testosterone. It acts synergistically with follicle-stimulating hormone (FSH).

Follicle-stimulating hormone (FSH) is a gonadotropin, a glycoprotein polypeptide hormone. FSH is synthesized and secreted by the gonadotropic cells of the anterior pituitary gland and regulates the development, growth, pubertal maturation, and reproductive processes of the body. FSH and luteinizing hormone (LH) work together in the reproductive system.

An ovarian cyst is a fluid-filled sac within the ovary. They usually cause no symptoms, but occasionally they may produce bloating, lower abdominal pain, or lower back pain. The majority of cysts are harmless. If the cyst either breaks open or causes twisting of the ovary, it may cause severe pain. This may result in vomiting or feeling faint, and even cause headaches.
The corpus luteum is a temporary endocrine structure in female ovaries involved in the production of relatively high levels of progesterone, and moderate levels of estradiol, and inhibin A. It is the remains of the ovarian follicle that has released a mature ovum during a previous ovulation.

The female reproductive system is made up of the internal and external sex organs that function in the reproduction of new offspring. The human female reproductive system is immature at birth and develops to maturity at puberty to be able to produce gametes, and to carry a fetus to full term. The internal sex organs are the vagina, uterus, fallopian tubes, and ovaries. The female reproductive tract includes the vagina, uterus, and fallopian tubes and is prone to infections. The vagina allows for sexual intercourse and childbirth, and is connected to the uterus at the cervix. The uterus or womb accommodates the embryo, which develops into the fetus. The uterus also produces secretions, which help the transit of sperm to the fallopian tubes, where sperm fertilize ova produced by the ovaries. The external sex organs are also known as the genitals and these are the organs of the vulva including the labia, clitoris, and vaginal opening.
Anovulation is when the ovaries do not release an oocyte during a menstrual cycle. Therefore, ovulation does not take place. However, a woman who does not ovulate at each menstrual cycle is not necessarily going through menopause. Chronic anovulation is a common cause of infertility.

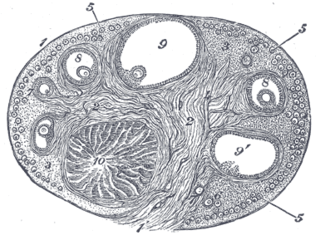
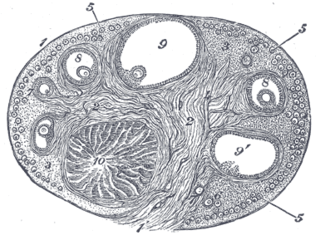
An ovarian follicle is a roughly spheroid cellular aggregation set found in the ovaries. It secretes hormones that influence stages of the menstrual cycle. At the time of puberty, women have approximately 200,000 to 300,000 follicles, each with the potential to release an egg cell (ovum) at ovulation for fertilization. These eggs are developed once every menstrual cycle with around 450–500 being ovulated during a woman's reproductive lifetime.

In biology, folliculogenesis is the maturation of the ovarian follicle, a densely packed shell of somatic cells that contains an immature oocyte. Folliculogenesis describes the progression of a number of small primordial follicles into large preovulatory follicles that occurs in part during the menstrual cycle.

The menstrual cycle is on average 28 days in length. It begins with menses during the follicular phase, followed by ovulation and ending with the luteal phase. Unlike the follicular phase which can vary in length among individuals, the luteal phase is typically fixed at approximately 14 days and is characterized by changes to hormone levels, such as an increase in progesterone and estrogen levels, decrease in gonadotropins such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH), changes to the endometrial lining to promote implantation of the fertilized egg, and development of the corpus luteum. In the absence of fertilization by sperm, the corpus luteum degenerates leading to a decrease in progesterone and estrogen, an increase in FSH and LH, and shedding of the endometrial lining (menses) to begin the menstrual cycle again.

The follicular phase, also known as the preovulatory phase or proliferative phase, is the phase of the estrous cycle during which follicles in the ovary mature from primary follicle to a fully mature graafian follicle. It ends with ovulation. The main hormones controlling this stage are secretion of gonadotropin-releasing hormones, which are follicle-stimulating hormones and luteinising hormones. They are released by pulsatile secretion. The duration of the follicular phase can differ depending on the length of the menstrual cycle, while the luteal phase is usually stable, does not really change and lasts 14 days.

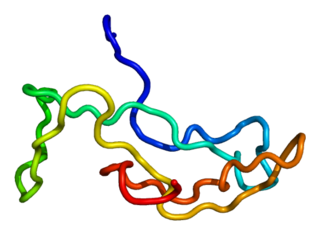
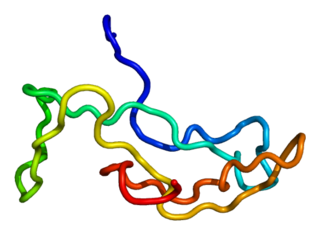
Bone morphogenetic protein 15 (BMP-15) is a protein that in humans is encoded by the BMP15 gene. It is involved in folliculogenesis, the process in which primordial follicles develop into pre-ovulatory follicles.
Ovulation induction is the stimulation of ovulation by medication. It is usually used in the sense of stimulation of the development of ovarian follicles to reverse anovulation or oligoovulation.

Ganirelix acetate, sold under the brand names Orgalutran and Antagon among others, is an injectable competitive gonadotropin-releasing hormone antagonist. It is primarily used in assisted reproduction to control ovulation. The drug works by blocking the action of gonadotropin-releasing hormone (GnRH) upon the pituitary, thus rapidly suppressing the production and action of LH and FSH. Ganirelix is used in fertility treatment to prevent premature ovulation that could result in the harvesting of eggs that are too immature to be used in procedures such as in vitro fertilization.
Ovarian diseases refer to diseases or disorders of the ovary.
Ovarian apoplexy is a sudden rupture in the ovary, commonly at the site of a cyst, accompanied by hemorrhage in the ovarian tissue and/or intraperitoneal bleeding.

Fertility testing is the process by which fertility is assessed, both generally and also to find the "fertile window" in the menstrual cycle. General health affects fertility, and STI testing is an important related field.
Ovarian follicle dominance is the process where one or more follicles are selected per cycle to ovulate.