The cervix or cervix uteri is the lower part of the uterus (womb) in the human female reproductive system. The cervix is usually 2 to 3 cm long and roughly cylindrical in shape, which changes during pregnancy. The narrow, central cervical canal runs along its entire length, connecting the uterine cavity and the lumen of the vagina. The opening into the uterus is called the internal os, and the opening into the vagina is called the external os. The lower part of the cervix, known as the vaginal portion of the cervix, bulges into the top of the vagina. The cervix has been documented anatomically since at least the time of Hippocrates, over 2,000 years ago.

In mammals, the vagina is the elastic, muscular part of the female genital tract. In humans, it extends from the vestibule to the cervix. The outer vaginal opening is normally partly covered by a thin layer of mucosal tissue called the hymen. At the deep end, the cervix bulges into the vagina. The vagina allows for sexual intercourse and birth. It also channels menstrual flow, which occurs in humans and closely related primates as part of the menstrual cycle.

Cervical cancer is a cancer arising from the cervix. It is due to the abnormal growth of cells that have the ability to invade or spread to other parts of the body. Early on, typically no symptoms are seen. Later symptoms may include abnormal vaginal bleeding, pelvic pain or pain during sexual intercourse. While bleeding after sex may not be serious, it may also indicate the presence of cervical cancer.
Gynecologic hemorrhage represents excessive bleeding of the female reproductive system. Such bleeding could be visible or external, namely bleeding from the vagina, or it could be internal into the pelvic cavity or form a hematoma. Normal menstruation is not considered a gynecologic hemorrhage, as it is not excessive. Hemorrhage associated with a pregnant state or during delivery is an obstetrical hemorrhage.

Hysterectomy is the surgical removal of the uterus and cervix. Supracervical hysterectomy refers to removal of the uterus while the cervix is spared. These procedures may also involve removal of the ovaries (oophorectomy), fallopian tubes (salpingectomy), and other surrounding structures. The term “partial” or “total” hysterectomy are lay-terms that incorrectly describe the addition or omission of oophorectomy at the time of hysterectomy. These procedures are usually performed by a gynecologist. Removal of the uterus renders the patient unable to bear children and has surgical risks as well as long-term effects, so the surgery is normally recommended only when other treatment options are not available or have failed. It is the second most commonly performed gynecological surgical procedure, after cesarean section, in the United States. Nearly 68 percent were performed for conditions such as endometriosis, irregular bleeding, and uterine fibroids. It is expected that the frequency of hysterectomies for non-malignant indications will continue to fall given the development of alternative treatment options.
A pessary is a prosthetic device inserted into the vagina for structural and pharmaceutical purposes. It is most commonly used to treat stress urinary incontinence to stop urinary leakage and to treat pelvic organ prolapse to maintain the location of organs in the pelvic region. It can also be used to administer medications locally in the vagina or as a method of contraception.
Heavy menstrual bleeding (HMB), previously known as menorrhagia or hematomunia, is a menstrual period with excessively heavy flow. It is a type of abnormal uterine bleeding (AUB).

Vaginal bleeding is any expulsion of blood from the vagina. This bleeding may originate from the uterus, vaginal wall, or cervix. Generally, it is either part of a normal menstrual cycle or is caused by hormonal or other problems of the reproductive system, such as abnormal uterine bleeding.
Antepartum bleeding, also known as antepartum haemorrhage (APH) or prepartum hemorrhage, is genital bleeding during pregnancy after the 28th week of pregnancy up to delivery.

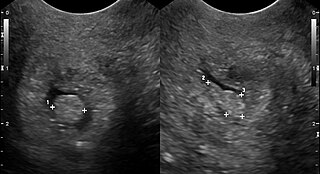
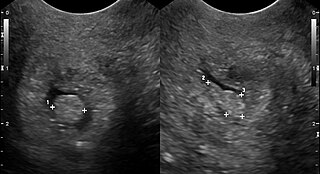
An endometrial polyp or uterine polyp is a mass in the inner lining of the uterus. They may have a large flat base (sessile) or be attached to the uterus by an elongated pedicle (pedunculated). Pedunculated polyps are more common than sessile ones. They range in size from a few millimeters to several centimeters. If pedunculated, they can protrude through the cervix into the vagina. Small blood vessels may be present, particularly in large polyps.
Bloody show or show is the passage of a small amount of blood or blood-tinged mucus through the vagina near the end of pregnancy. It is caused by thinning and dilation of the cervix, leading to detachment of the cervical mucus plug that seals the cervix during pregnancy and tearing of small cervical blood vessels, and is one of the signs that labor may be imminent. The bloody show may be expelled from the vagina in pieces or altogether and often appears as a jelly-like piece of mucus stained with blood. Although the bloody show may be alarming at first, it is not a concern of patient health after 37 weeks gestation.

Endometritis is inflammation of the inner lining of the uterus (endometrium). Symptoms may include fever, lower abdominal pain, and abnormal vaginal bleeding or discharge. It is the most common cause of infection after childbirth. It is also part of spectrum of diseases that make up pelvic inflammatory disease.
Intermenstrual bleeding (IMB) is vaginal bleeding at irregular intervals between expected menstrual periods. It may be associated with bleeding with sexual intercourse.

Vaginal discharge is a mixture of liquid, cells, and bacteria that lubricate and protect the vagina. This mixture is constantly produced by the cells of the vagina and cervix, and it exits the body through the vaginal opening. The composition, amount, and quality of discharge varies between individuals and can vary throughout the menstrual cycle and throughout the stages of sexual and reproductive development. Normal vaginal discharge may have a thin, watery consistency or a thick, sticky consistency, and it may be clear or white in color. Normal vaginal discharge may be large in volume but typically does not have a strong odor, nor is it typically associated with itching or pain. While most discharge is considered physiologic or represents normal functioning of the body, some changes in discharge can reflect infection or other pathological processes. Infections that may cause changes in vaginal discharge include vaginal yeast infections, bacterial vaginosis, and sexually transmitted infections. The characteristics of abnormal vaginal discharge vary depending on the cause, but common features include a change in color, a foul odor, and associated symptoms such as itching, burning, pelvic pain, or pain during sexual intercourse.
Vaginal cancer is an extraordinarily rare form of cancer that develops in the tissue of the vagina. Primary vaginal cancer originates from the vaginal tissue – most frequently squamous cell carcinoma, but primary vaginal adenocarcinoma, sarcoma, and melanoma have also been reported – while secondary vaginal cancer involves the metastasis of a cancer that originated in a different part of the body. Secondary vaginal cancer is more common. Signs of vaginal cancer may include abnormal vaginal bleeding, dysuria, tenesmus, or pelvic pain, though as many as 20% of women diagnosed with vaginal cancer are asymptomatic at the time of diagnosis. Vaginal cancer occurs more frequently in women over age 50, and the mean age of diagnosis of vaginal cancer is 60 years. It often can be cured if found and treated in early stages. Surgery alone or surgery combined with pelvic radiation is typically used to treat vaginal cancer.

A pelvic examination is the physical examination of the external and internal female pelvic organs. It is frequently used in gynecology for the evaluation of symptoms affecting the female reproductive and urinary tract, such as pain, bleeding, discharge, urinary incontinence, or trauma. It can also be used to assess a woman's anatomy in preparation for procedures. The exam can be done awake in the clinic and emergency department, or under anesthesia in the operating room. The most commonly performed components of the exam are 1) the external exam, to evaluate the external genitalia 2) the internal exam with palpation to examine the uterus, ovaries, and fallopian tubes, and 3) the internal exam using the speculum to visualize the vaginal walls and cervix. During the pelvic exam, sample of cells and fluids may be collected to screen for sexually transmitted infections or cancer.

The endometrial biopsy is a medical procedure that involves taking a tissue sample of the lining of the uterus. The tissue subsequently undergoes a histologic evaluation which aids the physician in forming a diagnosis.
A cervical polyp is a common benign polyp or tumour on the surface of the cervical canal. They can cause irregular menstrual bleeding but often show no symptoms. Treatment consists of simple removal of the polyp and prognosis is generally good. About 1% of cervical polyps will show neoplastic change which may lead to cancer. They are most common in post-menarche, pre-menopausal women who have been pregnant.
Female genital disease is a disorder of the structure or function of the female reproductive system that has a known cause and a distinctive group of symptoms, signs, or anatomical changes. The female reproductive system consists of the ovaries, fallopian tubes, uterus, vagina, and vulva. Female genital diseases can be classified by affected location or by type of disease, such as malformation, inflammation, or infection.
Early pregnancy bleeding refers to vaginal bleeding before 14 weeks of gestational age. If the bleeding is significant, hemorrhagic shock may occur. Concern for shock is increased in those who have loss of consciousness, chest pain, shortness of breath, or shoulder pain.