Arthroscopy is a minimally invasive surgical procedure on a joint in which an examination and sometimes treatment of damage is performed using an arthroscope, an endoscope that is inserted into the joint through a small incision. Arthroscopic procedures can be performed during ACL reconstruction.
A joint or articulation is the connection made between bones, ossicles, or other hard structures in the body which link an animal's skeletal system into a functional whole. They are constructed to allow for different degrees and types of movement. Some joints, such as the knee, elbow, and shoulder, are self-lubricating, almost frictionless, and are able to withstand compression and maintain heavy loads while still executing smooth and precise movements. Other joints such as sutures between the bones of the skull permit very little movement in order to protect the brain and the sense organs. The connection between a tooth and the jawbone is also called a joint, and is described as a fibrous joint known as a gomphosis. Joints are classified both structurally and functionally.

Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone which affects 1 in 7 adults in the United States. It is believed to be the fourth leading cause of disability in the world. The most common symptoms are joint pain and stiffness. Usually the symptoms progress slowly over years. Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs, the knee and hip joints, and the joints of the neck and lower back. The symptoms can interfere with work and normal daily activities. Unlike some other types of arthritis, only the joints, not internal organs, are affected.
An osteotomy is a surgical operation whereby a bone is cut to shorten or lengthen it or to change its alignment. It is sometimes performed to correct a hallux valgus, or to straighten a bone that has healed crookedly following a fracture. It is also used to correct a coxa vara, genu valgum, and genu varum. The operation is done under a general anaesthetic.
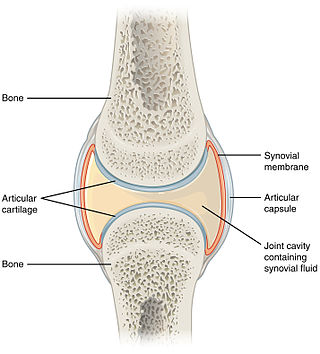
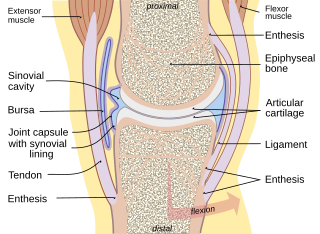
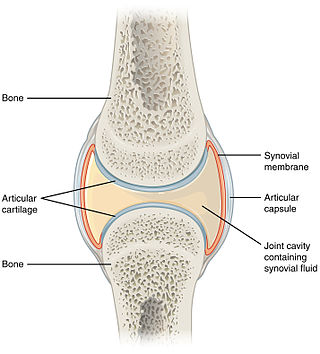
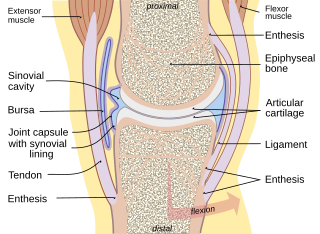
A synovial joint, also known as diarthrosis, joins bones or cartilage with a fibrous joint capsule that is continuous with the periosteum of the joined bones, constitutes the outer boundary of a synovial cavity, and surrounds the bones' articulating surfaces. This joint unites long bones and permits free bone movement and greater mobility. The synovial cavity/joint is filled with synovial fluid. The joint capsule is made up of an outer layer of fibrous membrane, which keeps the bones together structurally, and an inner layer, the synovial membrane, which seals in the synovial fluid.

Back injuries result from damage, wear, or trauma to the bones, muscles, or other tissues of the back. Common back injuries include sprains and strains, herniated discs, and fractured vertebrae. The lumbar spine is often the site of back pain. The area is susceptible because of its flexibility and the amount of body weight it regularly bears. It is estimated that low-back pain may affect as much as 80 to 90 percent of the general population in the United States.

Genu valgum, commonly called "knock-knee", is a condition in which the knees angle in and touch each other when the legs are straightened. Individuals with severe valgus deformities are typically unable to touch their feet together while simultaneously straightening the legs. The term originates from the Latin genu, 'knee', and valgus which means "bent outwards", but is also used to describe the distal portion of the knee joint which bends outwards and thus the proximal portion seems to be bent inwards.

Genu varum is a varus deformity marked by (outward) bowing at the knee, which means that the lower leg is angled inward (medially) in relation to the thigh's axis, giving the limb overall the appearance of an archer's bow. Usually medial angulation of both lower limb bones is involved.

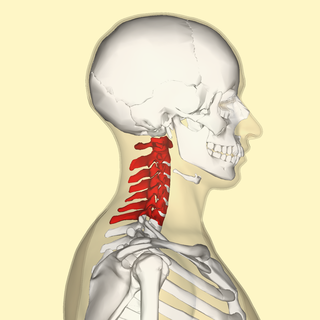
Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related degeneration of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.

A joint dislocation, also called luxation, occurs when there is an abnormal separation in the joint, where two or more bones meet. A partial dislocation is referred to as a subluxation. Dislocations are often caused by sudden trauma on the joint like an impact or fall. A joint dislocation can cause damage to the surrounding ligaments, tendons, muscles, and nerves. Dislocations can occur in any major joint or minor joint. The most common joint dislocation is a shoulder dislocation.
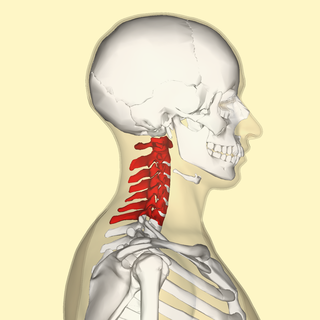
In tetrapods, cervical vertebrae are the vertebrae of the neck, immediately below the skull. Truncal vertebrae lie caudal of cervical vertebrae. In sauropsid species, the cervical vertebrae bear cervical ribs. In lizards and saurischian dinosaurs, the cervical ribs are large; in birds, they are small and completely fused to the vertebrae. The vertebral transverse processes of mammals are homologous to the cervical ribs of other amniotes. Most mammals have seven cervical vertebrae, with the only three known exceptions being the manatee with six, the two-toed sloth with five or six, and the three-toed sloth with nine.

Spondylolisthesis is the displacement of one spinal vertebra compared to another. While some medical dictionaries define spondylolisthesis specifically as the forward or anterior displacement of a vertebra over the vertebra inferior to it, it is often defined in medical textbooks as displacement in any direction. Spondylolisthesis is graded based upon the degree of slippage of one vertebral body relative to the subsequent adjacent vertebral body. Spondylolisthesis is classified as one of the six major etiologies: degenerative, traumatic, dysplastic, isthmic, pathologic, or post-surgical. Spondylolisthesis most commonly occurs in the lumbar spine, primarily at the L5-S1 level, with the L5 vertebral body anteriorly translating over the S1 vertebral body.
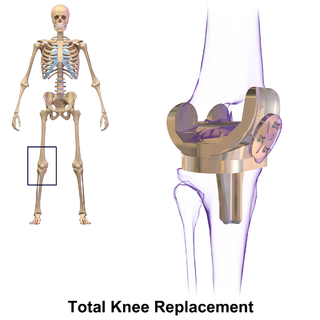
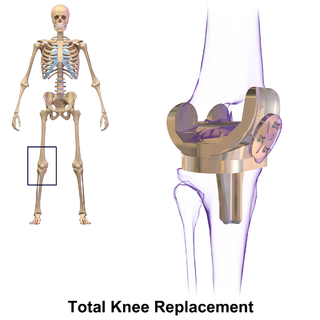
Knee replacement, also known as knee arthroplasty, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability, most commonly offered when joint pain is not diminished by conservative sources. It may also be performed for other knee diseases, such as rheumatoid arthritis. In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long-standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation, and is not a reason to perform knee replacement.
A meniscus transplant or meniscal transplant is a transplant of the meniscus of the knee, which separates the thigh bone (femur) from the lower leg bone (tibia). The worn or damaged meniscus is removed and is replaced with a new one from a donor. The meniscus to be transplanted is taken from a cadaver, and, as such, is known as an allograft. Meniscal transplantation is technically difficult, as it must be sized accurately for each person, positioned properly and secured to the tibial plateau. Its success also depends on donor compatibility, stability of the transplant, and long-term health of the underlying articular cartilage.
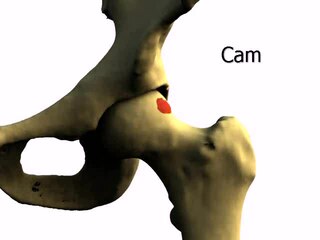
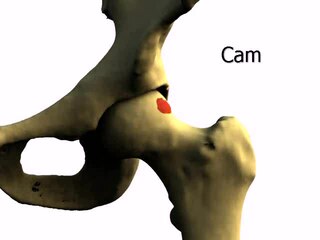
Femoroacetabular impingement (FAI) is a condition involving one or more anatomical abnormalities of the hip joint, which is a ball and socket joint. It is a common cause of hip pain and discomfort in young and middle-aged adults. It occurs when the ball shaped femoral head contacts the acetabulum abnormally or does not permit a normal range of motion in the acetabular socket. Damage can occur to the articular cartilage, or labral cartilage, or both. The condition may be symptomatic or asymptomatic. It may cause osteoarthritis of the hip. Treatment options range from conservative management to surgery.

Facet syndrome is a syndrome in which the facet joints cause painful symptoms. In conjunction with degenerative disc disease, a distinct but functionally related condition, facet arthropathy is believed to be one of the most common causes of lower back pain.

Diffuse idiopathic skeletal hyperostosis (DISH) is a condition characterized by abnormal calcification/bone formation (hyperostosis) of the soft tissues surrounding the joints of the spine, and also of the peripheral or appendicular skeleton. In the spine, there is bone formation along the anterior longitudinal ligament and sometimes the posterior longitudinal ligament, which may lead to partial or complete fusion of adjacent vertebrae. The facet and sacroiliac joints tend to be uninvolved. The thoracic spine is the most common level involved. In the peripheral skeleton, DISH manifests as a calcific enthesopathy, with pathologic bone formation at sites where ligaments and tendons attach to bone.

Spinal stenosis is an abnormal narrowing of the spinal canal or neural foramen that results in pressure on the spinal cord or nerve roots. Symptoms may include pain, numbness, or weakness in the arms or legs. Symptoms are typically gradual in onset and improve with leaning forward. Severe symptoms may include loss of bladder control, loss of bowel control, or sexual dysfunction.

Pain in the hip is the experience of pain in the muscles or joints in the hip/ pelvic region, a condition commonly arising from any of a number of factors. Sometimes it is closely associated with lower back pain.
X-ray motion analysis is a technique used to track the movement of objects using X-rays. This is done by placing the subject to be imaged in the center of the X-ray beam and recording the motion using an image intensifier and a high-speed camera, allowing for high quality videos sampled many times per second. Depending on the settings of the X-rays, this technique can visualize specific structures in an object, such as bones or cartilage. X-ray motion analysis can be used to perform gait analysis, analyze joint movement, or record the motion of bones obscured by soft tissue. The ability to measure skeletal motions is a key aspect to one's understanding of vertebrate biomechanics, energetics, and motor control.