Ataxia is a neurological sign consisting of lack of voluntary coordination of muscle movements that can include gait abnormality, speech changes, and abnormalities in eye movements, that indicates dysfunction of parts of the nervous system that coordinate movement, such as the cerebellum.

Myoclonus is a brief, involuntary, irregular twitching of a muscle, a joint, or a group of muscles, different from clonus, which is rhythmic or regular. Myoclonus describes a medical sign and, generally, is not a diagnosis of a disease. It belongs to the hyperkinetic movement disorders, among tremor and chorea for example. These myoclonic twitches, jerks, or seizures are usually caused by sudden muscle contractions or brief lapses of contraction. The most common circumstance under which they occur is while falling asleep. Myoclonic jerks occur in healthy people and are experienced occasionally by everyone. However, when they appear with more persistence and become more widespread they can be a sign of various neurological disorders. Hiccups are a kind of myoclonic jerk specifically affecting the diaphragm. When a spasm is caused by another person it is known as a provoked spasm. Shuddering attacks in babies fall in this category.

Dystonia is a neurological hyperkinetic movement disorder in which sustained or repetitive muscle contractions occur involuntarily, resulting in twisting and repetitive movements or abnormal fixed postures. The movements may resemble a tremor. Dystonia is often intensified or exacerbated by physical activity, and symptoms may progress into adjacent muscles.
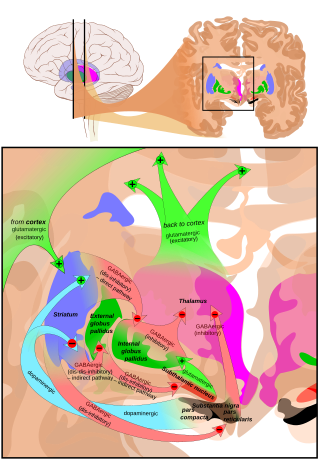
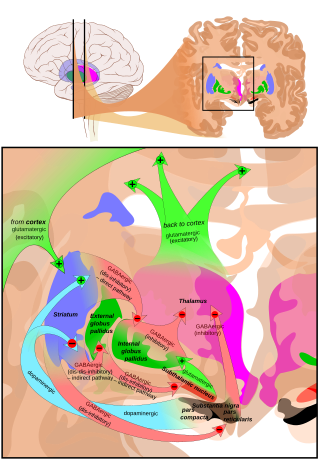
Hyperkinesia refers to an increase in muscular activity that can result in excessive abnormal movements, excessive normal movements, or a combination of both. Hyperkinesia is a state of excessive restlessness which is featured in a large variety of disorders that affect the ability to control motor movement, such as Huntington's disease. It is the opposite of hypokinesia, which refers to decreased bodily movement, as commonly manifested in Parkinson's disease.

Behr syndrome is characterized by the association of early-onset optic atrophy with spinocerebellar degeneration resulting in ataxia, pyramidal signs, peripheral neuropathy and developmental delay.
Cerebellar ataxia is a form of ataxia originating in the cerebellum. Non-progressive congenital ataxia (NPCA) is a classical presentation of cerebral ataxias.
Myoclonic epilepsy refers to a family of epilepsies that present with myoclonus. When myoclonic jerks are occasionally associated with abnormal brain wave activity, it can be categorized as myoclonic seizure. If the abnormal brain wave activity is persistent and results from ongoing seizures, then a diagnosis of myoclonic epilepsy may be considered.
Intention tremor is a dyskinetic disorder characterized by a broad, coarse, and low-frequency tremor evident during deliberate and visually-guided movement. An intention tremor is usually perpendicular to the direction of movement. When experiencing an intention tremor, one often overshoots or undershoots one's target, a condition known as dysmetria. Intention tremor is the result of dysfunction of the cerebellum, particularly on the same side as the tremor in the lateral zone, which controls visually guided movements. Depending on the location of cerebellar damage, these tremors can be either unilateral or bilateral.

MERRF syndrome is a mitochondrial disease. It is extremely rare, and has varying degrees of expressivity owing to heteroplasmy. MERRF syndrome affects different parts of the body, particularly the muscles and nervous system. The signs and symptoms of this disorder appear at an early age, generally childhood or adolescence. The causes of MERRF syndrome are difficult to determine, but because it is a mitochondrial disorder, it can be caused by the mutation of nuclear DNA or mitochondrial DNA. The classification of this disease varies from patient to patient, since many individuals do not fall into one specific disease category. The primary features displayed on a person with MERRF include myoclonus, seizures, cerebellar ataxia, myopathy, and ragged red fibers (RRF) on muscle biopsy, leading to the disease's name. Secondary features include dementia, optic atrophy, bilateral deafness, peripheral neuropathy, spasticity, or multiple lipomata. Mitochondrial disorders, including MERRFS, may present at any age.
Juvenile myoclonic epilepsy (JME), also known as Janz syndrome or impulsive petit mal, is a form of hereditary, idiopathic generalized epilepsy, representing 5–10% of all epilepsy cases. Typically it first presents between the ages of 12 and 18 with myoclonic seizures. These events typically occur after awakening from sleep, during the evening or when sleep-deprived. JME is also characterized by generalized tonic–clonic seizures, and a minority of patients have absence seizures. It was first described by Théodore Herpin in 1857. Understanding of the genetics of JME has been rapidly evolving since the 1990s, and over 20 chromosomal loci and multiple genes have been identified. Given the genetic and clinical heterogeneity of JME some authors have suggested that it should be thought of as a spectrum disorder.
Progressive Myoclonic Epilepsies (PME) are a rare group of inherited neurodegenerative diseases characterized by myoclonus, resistance to treatment, and neurological deterioration. The cause of PME depends largely on the type of PME. Most PMEs are caused by autosomal dominant or recessive and mitochondrial mutations. The location of the mutation also affects the inheritance and treatment of PME. Diagnosing PME is difficult due to their genetic heterogeneity and the lack of a genetic mutation identified in some patients. The prognosis depends largely on the worsening symptoms and failure to respond to treatment. There is no current cure for PME and treatment focuses on managing myoclonus and seizures through antiepileptic medication (AED).
Three different neurological syndromes carry the name of Ramsay Hunt syndrome. Their only connection is that they were all first documented by the famous neurologist James Ramsay Hunt (1872–1937).

Dentatorubral–pallidoluysian atrophy (DRPLA) is an autosomal dominant spinocerebellar degeneration caused by an expansion of a CAG repeat encoding a polyglutamine tract in the atrophin-1 protein. It is also known as Haw River Syndrome and Naito–Oyanagi disease. Although this condition was perhaps first described by Smith et al. in 1958, and several sporadic cases have been reported from Western countries, this disorder seems to be very rare except in Japan.
Benedikt syndrome, also called Benedikt's syndrome or paramedian midbrain syndrome, is a rare type of posterior circulation stroke of the brain, with a range of neurological symptoms affecting the midbrain, cerebellum and other related structures.

Spinal muscular atrophy with progressive myoclonic epilepsy (SMA-PME), sometimes called Jankovic–Rivera syndrome, is a very rare neurodegenerative disease whose symptoms include slowly progressive muscle (atrophy), predominantly affecting proximal muscles, combined with denervation and myoclonic seizures. Only 12 known human families are described in scientific literature to have SMA-PME.

Harding ataxia is an autosomal recessive cerebellar ataxia originally described by Harding in 1981. This form of cerebellar ataxia is similar to Friedreich ataxia including that it results in poor reflexes and balance, but differs in several ways, including the absence of diabetes mellitus, optic atrophy, cardiomyopathy, skeletal abnormalities, and the fact that tendon reflexes in the arms and knees remain intact. This form of ataxia is characterized by onset in the first 20 years, and is less severe than Friedreich ataxia. Additional cases were diagnosed in 1989, 1990, 1991, and 1998.
PRICKLE1-related progressive myoclonus epilepsy with ataxia is a very rare genetic disorder which is characterized by myoclonic epilepsy and ataxia.
Sensory ataxic neuropathy, dysarthria, and ophthalmoparesis, also known as SANDO syndrome, is a very rare genetic disorder which is characterized by ocular and nerve anomalies.
GOSR2-related progressive myoclonus ataxia, also known as Progressive myoclonic epilepsy type 6 is a rare genetic type of progressive myoclonus ataxia which is characterized by progressive myoclonic epilepsy with an early onset which is associated with generalized tonic-clonic seizures, petit mal seizures, and drop attacks, variable degrees of scoliosis, areflexia, high levels of creatine kinase serum, and late-onset cognitive decline.