Related Research Articles

Cardiomyopathy is a group of primary diseases of the heart muscle. Early on there may be few or no symptoms. As the disease worsens, shortness of breath, feeling tired, and swelling of the legs may occur, due to the onset of heart failure. An irregular heart beat and fainting may occur. Those affected are at an increased risk of sudden cardiac death.
Hypertrophic cardiomyopathy is a condition in which muscle tissues of the heart become thickened without an obvious cause. The parts of the heart most commonly affected are the interventricular septum and the ventricles. This results in the heart being less able to pump blood effectively and also may cause electrical conduction problems. Specifically, within the bundle branches that conduct impulses through the interventricular septum and into the Purkinje fibers, as these are responsible for the depolarization of contractile cells of both ventricles.

Ventricular hypertrophy (VH) is thickening of the walls of a ventricle of the heart. Although left ventricular hypertrophy (LVH) is more common, right ventricular hypertrophy (RVH), as well as concurrent hypertrophy of both ventricles can also occur.

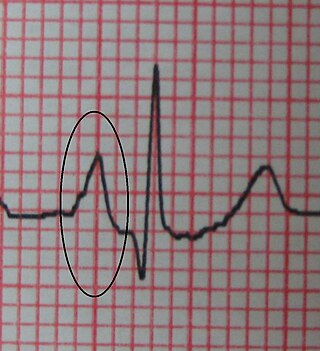
In cardiology, T wave alternans (TWA) is a periodic beat-to-beat variation in the amplitude or shape of the T wave in an electrocardiogram . TWA was first described in 1908. At that time, only large variations could be detected. Those large TWAs were associated with increased susceptibility to lethal ventricular tachycardias.

Cardiomegaly is a medical condition in which the heart becomes enlarged. It is more commonly referred to simply as "having an enlarged heart". It is usually the result of underlying conditions that make the heart work harder, such as obesity, heart valve disease, high blood pressure (hypertension), and coronary artery disease. Cardiomyopathy is also associated with cardiomegaly.

Disopyramide is an antiarrhythmic medication used in the treatment of ventricular tachycardia. It is a sodium channel blocker and is classified as a Class 1a anti-arrhythmic agent. Disopyramide has a negative inotropic effect on the ventricular myocardium, significantly decreasing the contractility. Disopyramide also has general anticholinergic effects which contribute to unwanted adverse effects. Disopyramide is available in both oral and intravenous forms. In 1972, when it was one of the only alternatives to quinidine, it was praised for being more potent and somewhat less toxic. However, a 2012 review of antiarrhythmic drugs noted that disopyramide is among the most toxic agents, with a high burden of side effects and increased mortality when used to treat atrial fibrillation.

Myocardial rupture is a laceration of the ventricles or atria of the heart, of the interatrial or interventricular septum, or of the papillary muscles. It is most commonly seen as a serious sequela of an acute myocardial infarction.
Alcohol septal ablation (ASA) is a minimally invasive heart procedure to treat hypertrophic cardiomyopathy (HCM).

Noncompaction cardiomyopathy (NCC) is a rare congenital disease of heart muscle that affects both children and adults. It results from abnormal prenatal development of heart muscle.
Alan W. Heldman is an American interventional cardiologist. Heldman graduated from Harvard College, University of Alabama School of Medicine, and completed residency and fellowship training at Johns Hopkins University School of Medicine. He held positions on the faculty of Johns Hopkins University from 1995 to 2007. In 2007, he became clinical chief of cardiology at the University of Miami's Miller School of Medicine.
Gerald Murray Lawrie is an American heart surgeon and pioneer in the surgical treatment of valvular heart disease of Australian descent.

Hypertrophic cardiomyopathy screening is an assessment and testing to detect hypertrophic cardiomyopathy (HCM).

Left atrial appendage occlusion (LAAO), also referred to as left atrial appendage closure (LAAC), is a procedure used to reduce the risk of blood clots from the left atrial appendage entering the bloodstream and causing a stroke in those with non-valvular atrial fibrillation.
Management of heart failure requires a multimodal approach. It involves a combination of lifestyle modifications, medications, and possibly the use of devices or surgery. It may be noted that treatment can vary across continents and regions.
Right atrial enlargement (RAE) is a form of cardiomegaly, or heart enlargement. It can broadly be classified as either right atrial hypertrophy (RAH), overgrowth, or dilation, like an expanding balloon. Common causes include pulmonary hypertension, which can be the primary defect leading to RAE, or pulmonary hypertension secondary to tricuspid stenosis; pulmonary stenosis or Tetralogy of Fallot i.e. congenital diseases; chronic lung disease, such as cor pulmonale. Other recognised causes are: right ventricular failure, tricuspid regurgitation, and atrial septal defect. Right atrial enlargement (RAE) is clinically significant due to its prevalence in diagnosing supraventricular arrhythmias. Further, early diagnosis using risk factors like RAE may decrease mortality because patients with RAE are at 9x more risk of arrhythmias and other cardiac conditions compared to their healthy counterparts. Treatment for RAE can include taking certain medications such as diuretics, beta-blockers, anticoagulants, and anti-arrhythmics. If medications are not effective enough, procedures such as implanting a pacemaker, cardioverter-defibrillator (ICD), or a left ventricular assist device (LVAD), heart valve surgery, and coronary bypass surgery may be needed. The last resort treatment option would be a complete heart transplant. Prevention for RAE comes from maintaining a healthy lifestyle with plenty of exercise and eating plenty of vegetables, fruits, and whole grains and avoiding or limiting alcohol and caffeine. It is also important to control heart disease risk factors including diabetes, high cholesterol, and high blood pressure. Exercise, pregnancy, and prior health conditions like ASD II can also promote cardiac remodeling, so routine primary care visits are important to distinguish between physiological and pathological atrial enlargement. Regular primary care visits and routine testing has also been shown to protect against the development of cardiovascular disease and may play a key role in early identification and treatment.
Ulrich Sigwart is a German retired cardiologist known for his pioneering role in the conception and clinical use of stents to keep blood vessels open, and introducing a non-surgical intervention, alcohol septal ablation for the treatment of hypertrophic obstructive cardiomyopathy.
Srihari S. Naidu is an American physician and Professor of Medicine at New York Medical College who is known for his work on hypertrophic cardiomyopathy including the procedure known as alcohol septal ablation, and for helping to construct the universal diagnostic criteria for cardiogenic shock.

Charles Knight is a British professor of cardiology and chief executive of St Bartholomew's Hospital, part of Barts Health NHS Trust.
Andrew G. Morrow , was chief of surgery at the National Heart Institute, who established the septal myectomy operation for obstructive hypertrophic cardiomyopathy (HCM). In 1960 he was part of the team that performed the first successful human mitral valve replacement using Nina Starr Braunwald's design.
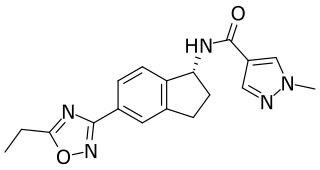
Aficamten (CK-274) is a cardiac myosin inhibitor developed by Cytokinetics for the treatment of obstructive hypertrophic cardiomyopathy.
References
- ↑ Cui, Hao; Schaff, Hartzell V. (2020). "80. Hypertrophic cardiomyopathy". In Raja, Shahzad G. (ed.). Cardiac Surgery: A Complete Guide. Switzerland: Springer. pp. 735–748. ISBN 978-3-030-24176-6.
- ↑ Ralph-Edwards, Anthony; Vanderlaan, Rachel D.; Bajona, Pietro (July 2017). "Transaortic septal myectomy: techniques and pitfalls". Annals of Cardiothoracic Surgery. 6 (4): 410–415. doi: 10.21037/acs.2017.07.08 . ISSN 2225-319X. PMC 5602211 . PMID 28944183.
- ↑ "History of Changes for Study: NCT04603521". clinicaltrials.gov. Retrieved 30 October 2022.
- ↑ Ommen S, Maron B, Olivotto I, Maron M, Cecchi F, Betocchi S, Gersh B, Ackerman M, McCully R, Dearani J, Schaff H, Danielson G, Tajik A, Nishimura R (2005). "Long-term effects of surgical septal myectomy on survival in patients with obstructive hypertrophic cardiomyopathy". J Am Coll Cardiol. 46 (3): 470–6. doi:10.1016/j.jacc.2005.02.090. PMID 16053960. S2CID 8546546.
- ↑ Ralph-Edwards A, Woo A, McCrindle B, Shapero J, Schwartz L, Rakowski H, Wigle E, Williams W (2005). "Hypertrophic obstructive cardiomyopathy: comparison of outcomes after myectomy or alcohol ablation adjusted by propensity score". J Thorac Cardiovasc Surg. 129 (2): 351–8. doi: 10.1016/j.jtcvs.2004.08.047 . PMID 15678046.
- ↑ Heldman AW, Wu KC, Abraham TP, Cameron DE (2007). "Myectomy or alcohol septal ablation surgery and percutaneous intervention go another round". J. Am. Coll. Cardiol. 49 (3): 358–60. doi:10.1016/j.jacc.2006.10.029. PMID 17239718.