Related Research Articles

Hyperthyroidism is the condition that occurs due to excessive production of thyroid hormones by the thyroid gland. Thyrotoxicosis is the condition that occurs due to excessive thyroid hormone of any cause and therefore includes hyperthyroidism. Some, however, use the terms interchangeably. Signs and symptoms vary between people and may include irritability, muscle weakness, sleeping problems, a fast heartbeat, heat intolerance, diarrhea, enlargement of the thyroid, hand tremor, and weight loss. Symptoms are typically less severe in the elderly and during pregnancy. An uncommon but life-threatening complication is thyroid storm in which an event such as an infection results in worsening symptoms such as confusion and a high temperature; this often results in death. The opposite is hypothyroidism, when the thyroid gland does not make enough thyroid hormone.
Kocher–Debré–Semelaigne syndrome(KDSS) is hypothyroidism in infancy or childhood characterised by lower extremity or generalized muscular hypertrophy (Herculean appearance), myxoedema, short stature, and cognitive impairment.

Lambert–Eaton myasthenic syndrome (LEMS) is a rare autoimmune disorder characterized by muscle weakness of the limbs.

Myasthenia gravis (MG) is a long-term neuromuscular junction disease that leads to varying degrees of skeletal muscle weakness. The most commonly affected muscles are those of the eyes, face, and swallowing. It can result in double vision, drooping eyelids, and difficulties in talking and walking. Onset can be sudden. Those affected often have a large thymus or develop a thymoma.

The thyroid, or thyroid gland, is an endocrine gland in vertebrates. In humans, it is in the neck and consists of two connected lobes. The lower two thirds of the lobes are connected by a thin band of tissue called the isthmus (pl.: isthmi). The thyroid gland is a butterfly-shaped gland located in the neck below the Adam's apple. Microscopically, the functional unit of the thyroid gland is the spherical thyroid follicle, lined with follicular cells (thyrocytes), and occasional parafollicular cells that surround a lumen containing colloid. The thyroid gland secretes three hormones: the two thyroid hormones – triiodothyronine (T3) and thyroxine (T4) – and a peptide hormone, calcitonin. The thyroid hormones influence the metabolic rate and protein synthesis and growth and development in children. Calcitonin plays a role in calcium homeostasis. Secretion of the two thyroid hormones is regulated by thyroid-stimulating hormone (TSH), which is secreted from the anterior pituitary gland. TSH is regulated by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus.

Graves' disease, also known as toxic diffuse goiter, is an autoimmune disease that affects the thyroid. It frequently results in and is the most common cause of hyperthyroidism. It also often results in an enlarged thyroid. Signs and symptoms of hyperthyroidism may include irritability, muscle weakness, sleeping problems, a fast heartbeat, poor tolerance of heat, diarrhea and unintentional weight loss. Other symptoms may include thickening of the skin on the shins, known as pretibial myxedema, and eye bulging, a condition caused by Graves' ophthalmopathy. About 25 to 30% of people with the condition develop eye problems.
Hypothyroidism is a disorder of the endocrine system in which the thyroid gland does not produce enough thyroid hormones. It can cause a number of symptoms, such as poor ability to tolerate cold, a feeling of tiredness, constipation, slow heart rate, depression, and weight gain. Occasionally there may be swelling of the front part of the neck due to goitre. Untreated cases of hypothyroidism during pregnancy can lead to delays in growth and intellectual development in the baby or congenital iodine deficiency syndrome.
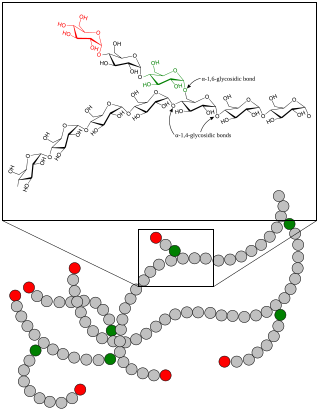
A glycogen storage disease is a metabolic disorder caused by a deficiency of an enzyme or transport protein affecting glycogen synthesis, glycogen breakdown, or glucose breakdown, typically in muscles and/or liver cells.
Weakness is a symptom of many different medical conditions. The causes are many and can be divided into conditions that have true or perceived muscle weakness. True muscle weakness is a primary symptom of a variety of skeletal muscle diseases, including muscular dystrophy and inflammatory myopathy. It occurs in neuromuscular junction disorders, such as myasthenia gravis.
In medicine, myopathy is a disease of the muscle in which the muscle fibers do not function properly. Myopathy means muscle disease. This meaning implies that the primary defect is within the muscle, as opposed to the nerves or elsewhere.

Exercise intolerance is a condition of inability or decreased ability to perform physical exercise at the normally expected level or duration for people of that age, size, sex, and muscle mass. It also includes experiences of unusually severe post-exercise pain, fatigue, nausea, vomiting or other negative effects. Exercise intolerance is not a disease or syndrome in and of itself, but can result from various disorders.
Nemaline myopathy is a congenital, often hereditary neuromuscular disorder with many symptoms that can occur such as muscle weakness, hypoventilation, swallowing dysfunction, and impaired speech ability. The severity of these symptoms varies and can change throughout one's life to some extent. The prevalence is estimated at 1 in 50,000 live births. It is the most common non-dystrophic myopathy.
Ocular myasthenia gravis (MG) is a disease of the neuromuscular junction resulting in hallmark variability in muscle weakness and fatigability. MG is an autoimmune disease where anomalous antibodies are produced against the naturally occurring acetylcholine receptors in voluntary muscles. MG may be limited to the muscles of the eye, leading to abrupt onset of weakness/fatigability of the eyelids or eye movement. MG may also involve other muscle groups.
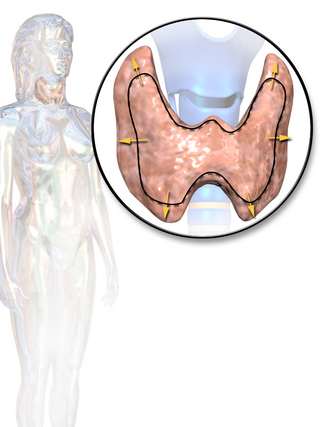
Thyroid disease is a medical condition that affects the function of the thyroid gland. The thyroid gland is located at the front of the neck and produces thyroid hormones that travel through the blood to help regulate many other organs, meaning that it is an endocrine organ. These hormones normally act in the body to regulate energy use, infant development, and childhood development.

Thyroiditis is the inflammation of the thyroid gland. The thyroid gland is located on the front of the neck below the laryngeal prominence, and makes hormones that control metabolism.
Muscle weakness is a lack of muscle strength. Its causes are many and can be divided into conditions that have either true or perceived muscle weakness. True muscle weakness is a primary symptom of a variety of skeletal muscle diseases, including muscular dystrophy and inflammatory myopathy. It occurs in neuromuscular junction disorders, such as myasthenia gravis. Muscle weakness can also be caused by low levels of potassium and other electrolytes within muscle cells. It can be temporary or long-lasting. The term myasthenia is from my- from Greek μυο meaning "muscle" + -asthenia ἀσθένεια meaning "weakness".

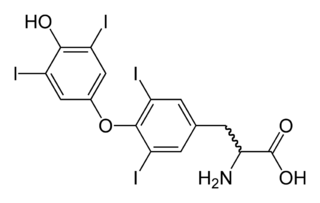
Thyroid hormones are any hormones produced and released by the thyroid gland, namely triiodothyronine (T3) and thyroxine (T4). They are tyrosine-based hormones that are primarily responsible for regulation of metabolism. T3 and T4 are partially composed of iodine, derived from food. A deficiency of iodine leads to decreased production of T3 and T4, enlarges the thyroid tissue and will cause the disease known as simple goitre.
Acquired non-inflammatory myopathy (ANIM) is a neuromuscular disorder primarily affecting skeletal muscle, most commonly in the limbs of humans, resulting in a weakness or dysfunction in the muscle. A myopathy refers to a problem or abnormality with the myofibrils, which compose muscle tissue. In general, non-inflammatory myopathies are a grouping of muscular diseases not induced by an autoimmune-mediated inflammatory pathway. These muscular diseases usually arise from a pathology within the muscle tissue itself rather than the nerves innervating that tissue. ANIM has a wide spectrum of causes which include drugs and toxins, nutritional imbalances, acquired metabolic dysfunctions such as an acquired defect in protein structure, and infections.

Thyrotoxic periodic paralysis (TPP) is a rare condition featuring attacks of muscle weakness in the presence of hyperthyroidism. Hypokalemia is usually present during attacks. The condition may be life-threatening if weakness of the breathing muscles leads to respiratory failure, or if the low potassium levels lead to abnormal heart rhythms. If untreated, it is typically recurrent in nature.
Amiodarone induced thyrotoxicosis (AIT) is a form of hyperthyroidism due to treatment with antiarrhythmic drug, amiodarone.
References
- 1 2 3 4 5 Kazakov, V.M., Terminal Intramuscular Motor Innervation and Motor End-Plates in Thyrotoxic Myopathy 2:343-349 (1992)
- ↑ Quinn EL, Worcester RL, Chronic thyrotoxic myopathy - report of a case. Journal of Clinical Endocrinology 11:1564-1571.1951.
- ↑ Horak HA, Pourmand R Endocrine myopathies. Neurologic Clinics 18:203-+ 2000.
- ↑ Kazakov VM. Differential-diagnosis of thyrotoxic myopathy. Klinicheskaya Meditsina 69:107-111 1991.
- ↑ Quinn EL, Worcester RL, Chronic thyrotoxic myopathy - report of a case. Journal of Clinical Endocrinology 11:1564-1571.1951.
- ↑ Lichtstein DM, Arteaga RB. Rhabdomyolysis associated with hyperthyroidism. American Journal of the Medical Sciences 332:103-105 2006
- ↑ 15. Olson BR, Klein I, Benner R, et al. Hyperthyroid myopathy and the response to treatment. Thyroid 1991;1:137-41.
- ↑ Rodolico C, Bonanno C, Pugliese A, Nicocia G, Benvenga S, Toscano A. Endocrine myopathies: clinical and histopathological features of the major forms. Acta Myol. 2020 Sep 1;39(3):130-135.
- ↑
- Kazakov VM, Katinas GS, Skorometz AA. Pathogenesis of experimental thyrotocis myopathy. European Neurology 25:212-224 1986
- ↑ Kazakov VM, Kovalenko TM. Experimental thyrotoxic myopathy - autoradiography of protein-synthesis in skeletal-muscle and motor-neurons of spinal-cord. Neuromuscular Disorders 5:47-52 1995.
- ↑ Chiu WY, Yang CC, Huang IC, Huang TS. Dysphagia as a manifestation of thyrotoxicosis: Report of three cases and literature review. Dysphagia 19:120-124 2004.
- ↑ Horak HA, Pourmand R Endocrine myopathies. Neurologic Clinics 18:203-+ 2000.
- ↑ Duyff, R., Bosch, J., Laman, D., Neuromuscular findings in Thyroid Dysfunction: a prospective clinical and electrodioagnostic study. Neural Neurosurg Psychiatry. 68:750-755. 2000
- ↑ Duyff, R., Bosch, J., Laman, D., Neuromuscular findings in Thyroid Dysfunction: a prospective clinical and electrodioagnostic study. Neural Neurosurg Psychiatry. 68:750-755. 2000