The kidneys are two bean-shaped organs found in vertebrates. They are located on the left and right in the retroperitoneal space, and in adult humans are about 12 centimetres (4.7 in) in length. They receive blood from the paired renal arteries; blood exits into the paired renal veins. Each kidney is attached to a ureter, a tube that carries excreted urine to the bladder.
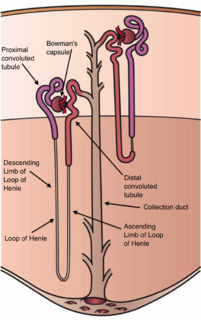
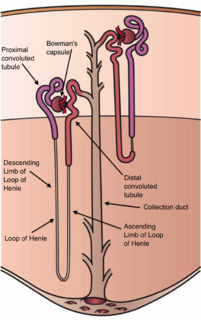
The nephron is the microscopic structural and functional unit of the kidney. It is composed of a renal corpuscle and a renal tubule. The renal corpuscle consists of a tuft of capillaries called a glomerulus and an encompassing Bowman's capsule. The renal tubule extends from the capsule. The capsule and tubule are connected and are composed of epithelial cells with a lumen. A healthy adult has 1 to 1.5 million nephrons in each kidney. Blood is filtered as it passes through three layers: the endothelial cells of the capillary wall, its basement membrane, and between the foot processes of the podocytes of the lining of the capsule. The tubule has adjacent peritubular capillaries that run between the descending and ascending portions of the tubule. As the fluid from the capsule flows down into the tubule, it is processed by the epithelial cells lining the tubule: water is reabsorbed and substances are exchanged ; first with the interstitial fluid outside the tubules, and then into the plasma in the adjacent peritubular capillaries through the endothelial cells lining that capillary. This process regulates the volume of body fluid as well as levels of many body substances. At the end of the tubule, the remaining fluid—urine—exits: it is composed of water, metabolic waste, and toxins.

The renin–angiotensin system (RAS), or renin–angiotensin–aldosterone system (RAAS), is a hormone system that regulates blood pressure and fluid and electrolyte balance, as well as systemic vascular resistance.

The juxtaglomerular apparatus is a structure in the kidney that regulates the function of each nephron, the functional units of the kidney. The juxtaglomerular apparatus is named because it is next to (juxta-) the glomerulus.
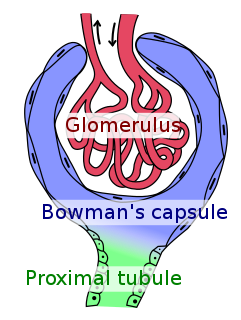
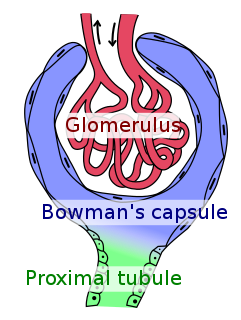
Bowman's capsule is a cup-like sack at the beginning of the tubular component of a nephron in the mammalian kidney that performs the first step in the filtration of blood to form urine. A glomerulus is enclosed in the sac. Fluids from blood in the glomerulus are collected in the Bowman's capsule.

Renal physiology is the study of the physiology of the kidney. This encompasses all functions of the kidney, including maintenance of acid-base balance; regulation of fluid balance; regulation of sodium, potassium, and other electrolytes; clearance of toxins; absorption of glucose, amino acids, and other small molecules; regulation of blood pressure; production of various hormones, such as erythropoietin; and activation of vitamin D.

A renal corpuscle is the blood-filtering component of the nephron of the kidney. It consists of a glomerulus - a tuft of capillaries composed of endothelial cells, and a glomerular capsule known as Bowman's capsule.

Renal function is an indication of the kidney's condition and its role in renal physiology. Glomerular filtration rate is a measure of kidney function.
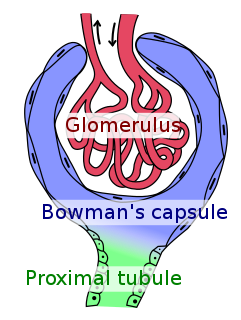
The glomerulus, is a network of small blood vessels (capillaries) known as a tuft, located at the beginning of a nephron in the kidney. The tuft is structurally supported by the mesangium - the space between the blood vessels - made up of intraglomerular mesangial cells. The blood is filtered across the capillary walls of this tuft through the glomerular filtration barrier, which yields its filtrate of water and soluble substances to a cup-like sac known as Bowman's capsule. The filtrate then enters the renal tubule of the nephron.

In the kidney, the macula densa is an area of closely packed specialized cells lining the wall of the distal tubule, at the point where the thick ascending limb of the Loop of Henle meets the distal convoluted tubule. The macula densa is the thickening where the distal tubule touches the glomerulus.
Mesangial cells are specialised cells in the kidney that make up the mesangium of the glomerulus. Together with the mesangial matrix, they form the vascular pole of the renal corpuscle. The mesangial cell population accounts for approximately 30-40% of the total cells in the glomerulus. Mesangial cells can be categorized as either extraglomerular mesangial cells or intraglomerular mesangial cells, based on their relative location to the glomerulus. The extraglomerular mesangial cells are found between the afferent and efferent arterioles towards the vascular pole of the glomerulus. The extraglomerular mesangial cells are adjacent to the intraglomerular mesangial cells that are located inside the glomerulus and in between the capillaries. The primary function of mesangial cells is to remove trapped residues and aggregated protein from the basement membrane thus keeping the filter free of debris. The contractile properties of mesangial cells have been shown to be insignificant in changing the filtration pressure of the glomerulus.

Podocytes are cells in the Bowman's capsule in the kidneys that wrap around capillaries of the glomerulus. Podocyte cells make up the epithelial lining of Bowman's capsule, the third layer through which filtration of blood takes place. The Bowman's capsule filters the blood, retaining large molecules such as proteins while smaller molecules such as water, salts, and sugars are filtered as the first step in the formation of urine. Although various viscera have epithelial layers, the name visceral epithelial cells usually refers specifically to podocytes, which are specialized epithelial cells that reside in the visceral layer of the capsule.
The Starling equation for fluid filtration is named for the British physiologist Ernest Starling, who is also recognised for the Frank–Starling law of the heart. The classic Starling equation has in recent years been revised. The Starling principle of fluid exchange is key to understanding how plasma fluid (solvent) within the bloodstream moves to the space outside the bloodstream. Starling can be credited with identifying that the "absorption of isotonic salt solutions by the blood vessels is determined by this osmotic pressure of the serum proteins." (1896)

Hypertensive kidney disease is a medical condition referring to damage to the kidney due to chronic high blood pressure. It manifests as hypertensive nephrosclerosis. It should be distinguished from renovascular hypertension, which is a form of secondary hypertension, and thus has opposite direction of causation.
Glycosuria is the excretion of glucose into the urine. Ordinarily, urine contains no glucose because the kidneys are able to reabsorb all of the filtered glucose from the tubular fluid back into the bloodstream. Glycosuria is nearly always caused by elevated blood glucose levels, most commonly due to untreated diabetes mellitus. Rarely, glycosuria is due to an intrinsic problem with glucose reabsorption within the kidneys, producing a condition termed renal glycosuria. Glycosuria leads to excessive water loss into the urine with resultant dehydration, a process called osmotic diuresis.

Hemofiltration, also haemofiltration, is a renal replacement therapy which is used in the intensive care setting. It is usually used to treat acute kidney injury (AKI), but may be of benefit in multiple organ dysfunction syndrome or sepsis. During hemofiltration, a patient's blood is passed through a set of tubing via a machine to a semipermeable membrane where waste products and water are removed by convection. Replacement fluid is added and the blood is returned to the patient.

The efferent arterioles are blood vessels that are part of the urinary tract of organisms. Efferent means "outgoing", in this case meaning carrying blood out away from the glomerulus. The efferent arterioles form from a convergence of the capillaries of the glomerulus, and carry blood away from the glomerulus that has already been filtered. They play an important role in maintaining the glomerular filtration rate despite fluctuations in blood pressure.
In renal physiology, reabsorption or tubular reabsorption is the process by which the nephron removes water and solutes from the tubular fluid (pre-urine) and returns them to the circulating blood. It is called reabsorption (and not absorption) both because these substances have already been absorbed once (particularly in the intestines) and because the body is reclaiming them from a postglomerular fluid stream that is well on its way to becoming urine (that is, they will soon be lost to the urine unless they are reclaimed). Substances are reabsorbed from the tubule into the peritubular capillaries. This happens as a result of sodium transport from the lumen into the blood by the Na+/K+ATPase in the basolateral membrane of the epithelial cells. Thus, the glomerular filtrate becomes more concentrated, which is one of the steps in forming urine. Reabsorption allows many useful solutes (primarily glucose and amino acids), salts and water that have passed through Bowman's capsule, to return to the circulation. These solutes are reabsorbed isotonically, in that the osmotic potential of the fluid leaving the proximal convoluted tubule is the same as that of the initial glomerular filtrate. However, glucose, amino acids, inorganic phosphate, and some other solutes are reabsorbed via secondary active transport through cotransport channels driven by the sodium gradient.
In the renal system, peritubular capillaries are tiny blood vessels, supplied by the efferent arteriole, that travel alongside nephrons allowing reabsorption and secretion between blood and the inner lumen of the nephron. Peritubular capillaries surround the cortical parts of the proximal and distal tubules, while the vasa recta go into the medulla to approach the loop of Henle.
In the physiology of the kidney, tubuloglomerular feedback (TGF) is a feedback system inside the kidneys. Within each nephron, information from the renal tubules is signaled to the glomerulus. Tubuloglomerular feedback is one of several mechanisms the kidney uses to regulate glomerular filtration rate (GFR). It involves the concept of purinergic signaling, in which an increased distal tubular sodium chloride concentration causes a basolateral release of adenosine from the macula densa cells. This initiates a cascade of events that ultimately brings GFR to an appropriate level.