A transient ischemic attack (TIA), commonly known as a mini-stroke, is a minor stroke whose noticeable symptoms usually end in less than an hour. TIA causes the same symptoms associated with strokes, such as weakness or numbness on one side of the body, sudden dimming or loss of vision, difficulty speaking or understanding language, slurred speech, or confusion.

Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders. The most common presentation of cerebrovascular disease is an ischemic stroke or mini-stroke and sometimes a hemorrhagic stroke. Hypertension is the most important contributing risk factor for stroke and cerebrovascular diseases as it can change the structure of blood vessels and result in atherosclerosis. Atherosclerosis narrows blood vessels in the brain, resulting in decreased cerebral perfusion. Other risk factors that contribute to stroke include smoking and diabetes. Narrowed cerebral arteries can lead to ischemic stroke, but continually elevated blood pressure can also cause tearing of vessels, leading to a hemorrhagic stroke.

Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue i.e. hypoxia and microvascular dysfunction. It also implies local hypoxia in a part of a body resulting from constriction. Ischemia causes not only insufficiency of oxygen, but also reduced availability of nutrients and inadequate removal of metabolic wastes. Ischemia can be partial or total blockage. The inadequate delivery of oxygenated blood to the organs must be resolved either by treating the cause of the inadequate delivery or reducing the oxygen demand of the system that needs it. For example, patients with myocardial ischemia have a decreased blood flow to the heart and are prescribed with medications that reduce chronotrophy and ionotrophy to meet the new level of blood delivery supplied by the stenosed vasculature so that it is adequate.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.

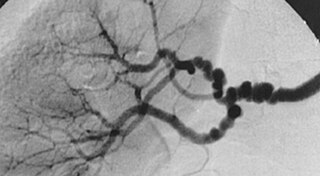
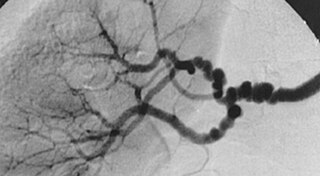
Cerebral angiography is a form of angiography which provides images of blood vessels in and around the brain, thereby allowing detection of abnormalities such as arteriovenous malformations and aneurysms. It was pioneered in 1927 by the Portuguese neurologist Egas Moniz at the University of Lisbon, who also helped develop thorotrast for use in the procedure.
A thunderclap headache is a headache that is severe and has a sudden onset. It is defined as a severe headache that takes seconds to minutes to reach maximum intensity. Although approximately 75% are attributed to "primary" headaches—headache disorder, non-specific headache, idiopathic thunderclap headache, or uncertain headache disorder—the remainder are secondary to other causes, which can include some extremely dangerous acute conditions, as well as infections and other conditions. Usually, further investigations are performed to identify the underlying cause.

Moyamoya disease is a disease in which certain arteries in the brain are constricted. Blood flow is blocked by constriction and blood clots (thrombosis). A collateral circulation develops around the blocked vessels to compensate for the blockage, but the collateral vessels are small, weak, and prone to bleeding, aneurysm and thrombosis. On conventional angiography, these collateral vessels have the appearance of a "puff of smoke".

Carotid endarterectomy is a surgical procedure used to reduce the risk of stroke from carotid artery stenosis. In endarterectomy, the surgeon opens the artery and removes the plaque. The plaque forms and thickens the inner layer of the artery, or intima, hence the name of the procedure which simply means removal of part of the internal layers of the artery.

Carotid artery stenosis is a narrowing or constriction of any part of the carotid arteries, usually caused by atherosclerosis.

Cerebral infarction is the pathologic process that results in an area of necrotic tissue in the brain. It is caused by disrupted blood supply (ischemia) and restricted oxygen supply (hypoxia), most commonly due to thromboembolism, and manifests clinically as ischemic stroke. In response to ischemia, the brain degenerates by the process of liquefactive necrosis.
Vertebrobasilar insufficiency (VBI) describes a temporary set of symptoms due to decreased blood flow (ischemia) in the posterior circulation of the brain. The posterior circulation supplies the medulla, pons, midbrain, cerebellum and supplies the posterior cerebellar artery to the thalamus and occipital cortex. As a result, symptoms vary widely depending which brain region is predominantly affected.

A watershed stroke is defined as a brain ischemia that is localized to the vulnerable border zones between the tissues supplied by the anterior, posterior and middle cerebral arteries. The actual blood stream blockage/restriction site can be located far away from the infarcts. Watershed locations are those border-zone regions in the brain supplied by the major cerebral arteries where blood supply is decreased. Watershed strokes are a concern because they comprise approximately 10% of all ischemic stroke cases. The watershed zones themselves are particularly susceptible to infarction from global ischemia as the distal nature of the vasculature predisposes these areas to be most sensitive to profound hypoperfusion.
Fibromuscular dysplasia (FMD) is a non-atherosclerotic, non-inflammatory disease of the blood vessels that causes abnormal growth within the wall of an artery. FMD has been found in nearly every arterial bed in the body, although the most commonly affected are the renal and carotid arteries.

Vertebral artery dissection (VAD) is a flap-like tear of the inner lining of the vertebral artery, which is located in the neck and supplies blood to the brain. After the tear, blood enters the arterial wall and forms a blood clot, thickening the artery wall and often impeding blood flow. The symptoms of vertebral artery dissection include head and neck pain and intermittent or permanent stroke symptoms such as difficulty speaking, impaired coordination, and visual loss. It is usually diagnosed with a contrast-enhanced CT or MRI scan.

Carotid artery stenting is an endovascular procedure where a stent is deployed within the lumen of the carotid artery to treat narrowing of the carotid artery and decrease the risk of stroke. It is used to treat narrowing of the carotid artery in high-risk patients, when carotid endarterectomy is considered too risky.

Eagle syndrome is an uncommon condition commonly characterized but not limited to sudden, sharp nerve-like pain in the jaw bone and joint, back of the throat, and base of the tongue, triggered by swallowing, moving the jaw, or turning the neck. First described by American otorhinolaryngologist Watt Weems Eagle in 1937, the condition is caused by an elongated or misshapen styloid process and/or calcification of the stylohyoid ligament, either of which interferes with the functioning of neighboring regions in the body, such as the glossopharyngeal nerve.
Ocular ischemic syndrome is the constellation of ocular signs and symptoms secondary to severe, chronic arterial hypoperfusion to the eye. Amaurosis fugax is a form of acute vision loss caused by reduced blood flow to the eye; it may be a warning sign of an impending stroke, as both stroke and retinal artery occlusion can be caused by thromboembolism due to atherosclerosis elsewhere in the body. Consequently, those with transient blurring of vision are advised to urgently seek medical attention for a thorough evaluation of the carotid artery. Anterior segment ischemic syndrome is a similar ischemic condition of anterior segment usually seen in post-surgical cases. Retinal artery occlusion leads to rapid death of retinal cells, thereby resulting in severe loss of vision.

Lacunar stroke or lacunar cerebral infarct (LACI) is the most common type of ischemic stroke, resulting from the occlusion of small penetrating arteries that provide blood to the brain's deep structures. Patients who present with symptoms of a lacunar stroke, but who have not yet had diagnostic imaging performed, may be described as having lacunar stroke syndrome (LACS).

Cervical artery dissection is dissection of one of the layers that compose the carotid and vertebral artery in the neck (cervix). They include:

Posterior spinal artery syndrome(PSAS), also known as posterior spinal cord syndrome, is a type of incomplete spinal cord injury. PSAS is the least commonly occurring of the six clinical spinal cord injury syndromes, with an incidence rate of less than 1%.