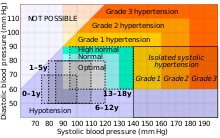
Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms itself. It is, however, a major risk factor for stroke, coronary artery disease, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia. Hypertension is a major cause of premature death worldwide.
Orthostatic hypotension, also known as postural hypotension, is a medical condition wherein a person's blood pressure drops when standing up or sitting down. Primary orthostatic hypotension is also often referred to as neurogenic orthostatic hypotension. The drop in blood pressure may be sudden, within 3 minutes or gradual. It is defined as a fall in systolic blood pressure of at least 20 mmHg or diastolic blood pressure of at least 10 mmHg after 3 minutes of standing. It occurs predominantly by delayed constriction of the lower body blood vessels, which is normally required to maintain adequate blood pressure when changing the position to standing. As a result, blood pools in the blood vessels of the legs for a longer period, and less is returned to the heart, thereby leading to a reduced cardiac output and inadequate blood flow to the brain.
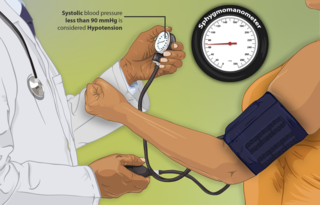
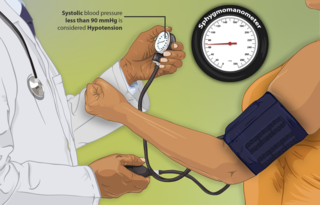
Hypotension, also known as low blood pressure, is a cardiovascular condition characterized by abnormally reduced blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood and is indicated by two numbers, the systolic blood pressure and the diastolic blood pressure, which are the maximum and minimum blood pressures within the cardiac cycle, respectively. A systolic blood pressure of less than 90 millimeters of mercury (mmHg) or diastolic of less than 60 mmHg is generally considered to be hypotension. Different numbers apply to children. However, in practice, blood pressure is considered too low only if noticeable symptoms are present.

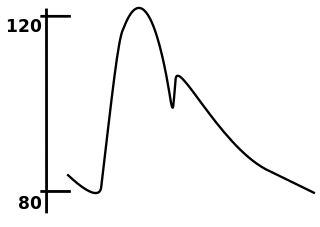
Pulse pressure is the difference between systolic and diastolic blood pressure. It is measured in millimeters of mercury (mmHg). It represents the force that the heart generates each time it contracts. Healthy pulse pressure is around 40 mmHg. A pulse pressure that is consistently 60 mmHg or greater is likely to be associated with disease, and a pulse pressure of 50 mmHg or more increases the risk of cardiovascular disease. Pulse pressure is considered low if it is less than 25% of the systolic. A very low pulse pressure can be a symptom of disorders such as congestive heart failure.

Afterload is the pressure that the heart must work against to eject blood during systole. Afterload is proportional to the average arterial pressure. As aortic and pulmonary pressures increase, the afterload increases on the left and right ventricles respectively. Afterload changes to adapt to the continually changing demands on an animal's cardiovascular system. Afterload is proportional to mean systolic blood pressure and is measured in millimeters of mercury.

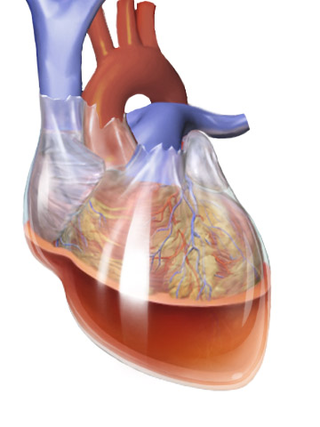
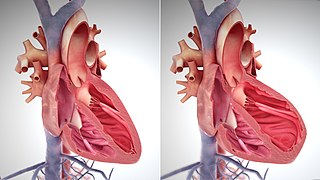
Aortic regurgitation (AR), also known as aortic insufficiency (AI), is the leaking of the aortic valve of the heart that causes blood to flow in the reverse direction during ventricular diastole, from the aorta into the left ventricle. As a consequence, the cardiac muscle is forced to work harder than normal.
Essential hypertension is a form of hypertension without an identifiable physiologic cause. It is the most common type affecting 85% of those with high blood pressure. The remaining 15% is accounted for by various causes of secondary hypertension. Essential hypertension tends to be familial and is likely to be the consequence of an interaction between environmental and genetic factors. Hypertension can increase the risk of cerebral, cardiac, and renal events.
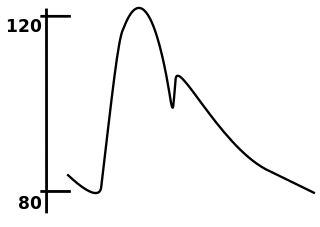
In medicine, the mean arterial pressure (MAP) is an average calculated blood pressure in an individual during a single cardiac cycle. Although methods of estimating MAP vary, a common calculation is to take one-third of the pulse pressure, and add that amount to the diastolic pressure. A normal MAP is about 90 mmHg.
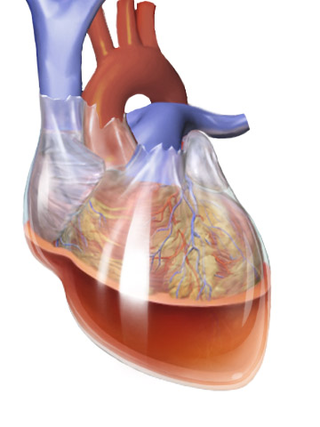
Beck's triad is a collection of three medical signs associated with acute cardiac tamponade, a medical emergency when excessive fluid accumulates in the pericardial sac around the heart and impairs its ability to pump blood. The signs are low arterial blood pressure, distended neck veins, and distant, muffled heart sounds.

A hypertensive emergency is very high blood pressure with potentially life-threatening symptoms and signs of acute damage to one or more organ systems. It is different from a hypertensive urgency by this additional evidence for impending irreversible hypertension-mediated organ damage (HMOD). Blood pressure is often above 200/120 mmHg, however there are no universally accepted cutoff values.
Pulsus paradoxus, also paradoxic pulse or paradoxical pulse, is an abnormally large decrease in stroke volume, systolic blood pressure and pulse wave amplitude during inspiration. Pulsus paradoxus is not related to pulse rate or heart rate, and it is not a paradoxical rise in systolic pressure. Normally, blood pressure drops less precipitously than 10 mmHg during inhalation. Pulsus paradoxus is a sign that is indicative of several conditions, most commonly pericardial effusion.
Cardiovascular physiology is the study of the cardiovascular system, specifically addressing the physiology of the heart ("cardio") and blood vessels ("vascular").
Arterial stiffness occurs as a consequence of biological aging and arteriosclerosis. Inflammation plays a major role in arteriosclerosis development, and consequently it is a major contributor in large arteries stiffening. Increased arterial stiffness is associated with an increased risk of cardiovascular events such as myocardial infarction, hypertension, heart failure and stroke, the two leading causes of death in the developed world. The World Health Organization predicts that in 2010, cardiovascular disease will also be the leading killer in the developing world and represents a major global health problem.
In medicine, systolic hypertension is defined as an elevated systolic blood pressure (SBP). If the systolic blood pressure is elevated (>140) with a normal (<90) diastolic blood pressure (DBP), it is called isolated systolic hypertension. Eighty percent of people with systolic hypertension are over the age of 65 years old. Isolated systolic hypertension is a specific type of widened pulse pressure.
Prehypertension, also known as high normal blood pressure and borderline hypertensive (BH), is a medical classification for cases where a person's blood pressure is elevated above optimal or normal, but not to the level considered hypertension. Prehypertension is now referred to as "elevated blood pressure" by the American College of Cardiology (ACC) and the American Heart Association (AHA). The ACC/AHA define elevated blood pressure as readings with a systolic pressure from 120 to 129 mm Hg and a diastolic pressure under 80 mm Hg, Readings greater than or equal to 130/80 mm Hg are considered hypertension by ACC/AHA and if greater than or equal to 140/90 mm Hg by ESC/ESH. and the European Society of Hypertension defines "high normal blood pressure" as readings with a systolic pressure from 130 to 139 mm Hg and a diastolic pressure 85-89 mm Hg.

Pathophysiology is a study which explains the function of the body as it relates to diseases and conditions. The pathophysiology of hypertension is an area which attempts to explain mechanistically the causes of hypertension, which is a chronic disease characterized by elevation of blood pressure. Hypertension can be classified by cause as either essential or secondary. About 90–95% of hypertension is essential hypertension. Some authorities define essential hypertension as that which has no known explanation, while others define its cause as being due to overconsumption of sodium and underconsumption of potassium. Secondary hypertension indicates that the hypertension is a result of a specific underlying condition with a well-known mechanism, such as chronic kidney disease, narrowing of the aorta or kidney arteries, or endocrine disorders such as excess aldosterone, cortisol, or catecholamines. Persistent hypertension is a major risk factor for hypertensive heart disease, coronary artery disease, stroke, aortic aneurysm, peripheral artery disease, and chronic kidney disease.

Orthostatic hypertension is a medical condition consisting of a sudden and abrupt increase in blood pressure (BP) when a person stands up. Orthostatic hypertension is diagnosed by a rise in systolic BP of 20 mmHg or more when standing. Orthostatic diastolic hypertension is a condition in which the diastolic BP raises to 98 mmHg or over in response to standing, but this definition currently lacks clear medical consensus, so is subject to change. Orthostatic hypertension involving the systolic BP is known as systolic orthostatic hypertension.

Heart failure with preserved ejection fraction (HFpEF) is a form of heart failure in which the ejection fraction – the percentage of the volume of blood ejected from the left ventricle with each heartbeat divided by the volume of blood when the left ventricle is maximally filled – is normal, defined as greater than 50%; this may be measured by echocardiography or cardiac catheterization. Approximately half of people with heart failure have preserved ejection fraction, while the other half have a reduction in ejection fraction, called heart failure with reduced ejection fraction (HFrEF).

Arterial blood pressure is most commonly measured via a sphygmomanometer, which historically used the height of a column of mercury to reflect the circulating pressure. Blood pressure values are generally reported in millimetres of mercury (mmHg), though aneroid and electronic devices do not contain mercury.
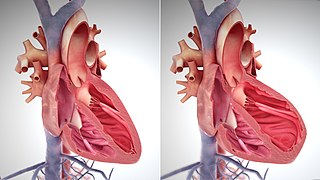
The main pathophysiology of heart failure is a reduction in the efficiency of the heart muscle, through damage or overloading. As such, it can be caused by a wide number of conditions, including myocardial infarction, hypertension and cardiac amyloidosis. Over time these increases in workload will produce changes to the heart itself: