The cervix or cervix uteri is the lower part of the uterus (womb) in the human female reproductive system. The cervix is usually 2 to 3 cm long and roughly cylindrical in shape, which changes during pregnancy. The narrow, central cervical canal runs along its entire length, connecting the uterine cavity and the lumen of the vagina. The opening into the uterus is called the internal os, and the opening into the vagina is called the external os. The lower part of the cervix, known as the vaginal portion of the cervix, bulges into the top of the vagina. The cervix has been documented anatomically since at least the time of Hippocrates, over 2,000 years ago.

The Papanicolaou test is a method of cervical screening used to detect potentially precancerous and cancerous processes in the cervix or colon. Abnormal findings are often followed up by more sensitive diagnostic procedures and, if warranted, interventions that aim to prevent progression to cervical cancer. The test was independently invented in the 1920s by the Greek physician Georgios Papanikolaou and named after him. A simplified version of the test was introduced by the Canadian obstetrician Anna Marion Hilliard in 1957.

Cervical cancer is a cancer arising from the cervix. It is due to the abnormal growth of cells that have the ability to invade or spread to other parts of the body. Early on, typically no symptoms are seen. Later symptoms may include abnormal vaginal bleeding, pelvic pain or pain during sexual intercourse. While bleeding after sex may not be serious, it may also indicate the presence of cervical cancer.
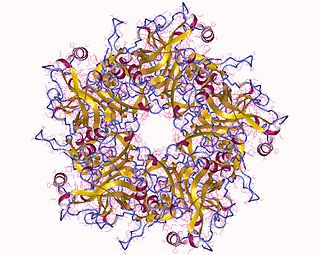
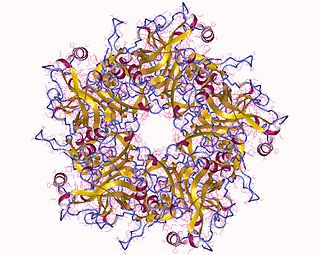
Human papillomavirus infection is caused by a DNA virus from the Papillomaviridae family. Many HPV infections cause no symptoms and 90% resolve spontaneously within two years. In some cases, an HPV infection persists and results in either warts or precancerous lesions. These lesions, depending on the site affected, increase the risk of cancer of the cervix, vulva, vagina, penis, anus, mouth, tonsils, or throat. Nearly all cervical cancer is due to HPV and two strains – HPV16 and HPV18 – which account for 70% of cases. HPV16 is responsible for almost 90% of HPV-positive oropharyngeal cancers. Between 60% and 90% of the other cancers listed above are also linked to HPV. HPV6 and HPV11 are common causes of genital warts and laryngeal papillomatosis.

Cytopathology is a branch of pathology that studies and diagnoses diseases on the cellular level. The discipline was founded by George Nicolas Papanicolaou in 1928. Cytopathology is generally used on samples of free cells or tissue fragments, in contrast to histopathology, which studies whole tissues. Cytopathology is frequently, less precisely, called "cytology", which means "the study of cells".

Colposcopy is a medical diagnostic procedure to visually examine the cervix as well as the vagina and vulva using a colposcope. Numbing should be requested prior to procedure.

Anal cancer is a cancer which arises from the anus, the distal opening of the gastrointestinal tract. Symptoms may include bleeding from the anus or a lump near the anus. Other symptoms may include pain, itchiness, or discharge from the anus. A change in bowel movements may also occur.

Cervical intraepithelial neoplasia (CIN), also known as cervical dysplasia, is the abnormal growth of cells on the surface of the cervix that could potentially lead to cervical cancer. More specifically, CIN refers to the potentially precancerous transformation of cells of the cervix.

A koilocyte is a squamous epithelial cell that has undergone a number of structural changes, which occur as a result of infection of the cell by human papillomavirus (HPV). Identification of these cells by pathologists can be useful in diagnosing various HPV-associated lesions.
Vaginal cancer is an extraordinarily rare form of cancer that develops in the tissue of the vagina. Primary vaginal cancer originates from the vaginal tissue – most frequently squamous cell carcinoma, but primary vaginal adenocarcinoma, sarcoma, and melanoma have also been reported – while secondary vaginal cancer involves the metastasis of a cancer that originated in a different part of the body. Secondary vaginal cancer is more common. Signs of vaginal cancer may include abnormal vaginal bleeding, dysuria, tenesmus, or pelvic pain, though as many as 20% of women diagnosed with vaginal cancer are asymptomatic at the time of diagnosis. Vaginal cancer occurs more frequently in women over age 50, and the mean age of diagnosis of vaginal cancer is 60 years. It often can be cured if found and treated in early stages. Surgery alone or surgery combined with pelvic radiation is typically used to treat vaginal cancer.
Colin Robert Andrew Laverty was an Australian medical practitioner and was the first to confirm that the human papillomavirus was much more common in the cervix than previously thought and, in 1978, he suggested that this virus be considered as possibly involved in the causation of cervical cancer. He was also a prolific art collector.
HspE7 is an investigational therapeutic vaccine candidate being developed by Nventa Biopharmaceuticals for the treatment of precancerous and cancerous lesions caused by the human papillomavirus (HPV). HspE7 uses recombinant DNA technology to covalently fuse a heat shock protein (Hsp) to a target antigen, thereby stimulating cellular immune system responses to specific diseases. HspE7 is a patented construct consisting of the HPV Type 16 E7 protein and heat shock protein 65 (Hsp65) and is currently the only candidate using Hsp technology to target the over 20 million Americans already infected with HPV.
An anal Pap smear is the anal counterpart of the cervical Pap smear. It is used for the early detection of anal cancer. Some types of human papillomavirus (HPV) can cause anal cancer. Other HPV types cause anogenital warts. Cigarette smokers, men who have sex with men, individuals with a history of immunosuppression and women with a history of cervical, vaginal and vulval cancer are at increased risk of getting anal cancer. Vaccination against HPV before initial sexual exposure can reduce the risk of anal cancer.
The Bethesda system (TBS), officially called The Bethesda System for Reporting Cervical Cytology, is a system for reporting cervical or vaginal cytologic diagnoses, used for reporting Pap smear results. It was introduced in 1988 and revised in 1991, 2001, and 2014. The name comes from the location of the conference, sponsored by the National Institutes of Health, that established the system.
Cervicography is a diagnostic medical procedure in which a non-physician takes pictures of the cervix and submits them to a physician for interpretation. Other related procedures are speculoscopy and colposcopy. The procedure is considered a screening test for cervical cancer and is complementary to Pap smear. The technique was initially developed by Adolf Stafl, MD, of Medical College of Wisconsin in 1981.

Liquid-based cytology is a method of preparing samples for examination in cytopathology. The sample is collected, normally by a small brush, in the same way as for a conventional smear test, but rather than the smear being transferred directly to a microscope slide, the sample is deposited into a small bottle of preservative liquid. At the laboratory, the liquid is treated to remove other elements such as mucus before a layer of cells is placed on a slide.
A well-woman examination is an exam offered to women to review elements of their reproductive health. The exam includes a breast examination, a pelvic examination and a Pap smear but may include other procedures. Hospitals employ strict policies relating to the provision of consent by the patient, the availability of chaperones at the examination, and the absence of other parties.
Microglandular hyperplasia (MGH) of the cervix is an epithelial benign abnormality (lesion) associated with gland proliferation. It can terminate in mature squamous metaplasia, and it is suspected reserve cells are involved in this process, perhaps in the form of reserve cell hyperplasia with glandular differentiation.

Gynecologic cancer disparities in the United States refer to differences in incidence, prevalence, and mortality from gynecologic cancers between population groups. The five main types of gynecologic cancer include cervical cancer, ovarian cancer, endometrial cancer, vaginal cancer, and vulvar cancer. For patients with these and other gynecologic malignancies within the United States, disparities across the care continuum by socioeconomic status and racial/ethnic background have been previously identified and studied. The causes behind these disparities are multifaceted and a complex interplay of systemic differences in health as well as individual patient factors such as cultural, educational, and economic barriers.
Pamela Toliman is a medical researcher from Papua New Guinea (PNG) who has researched areas such as sexually transmitted diseases, HIV/AIDS, cervical cancer and COVID-19.