Hysterectomy is the surgical removal of the uterus and cervix. Supracervical hysterectomy refers to removal of the uterus while the cervix is spared. These procedures may also involve removal of the ovaries (oophorectomy), fallopian tubes (salpingectomy), and other surrounding structures. The term “partial” or “total” hysterectomy are lay-terms that incorrectly describe the addition or omission of oophorectomy at the time of hysterectomy. These procedures are usually performed by a gynecologist. Removal of the uterus renders the patient unable to bear children and has surgical risks as well as long-term effects, so the surgery is normally recommended only when other treatment options are not available or have failed. It is the second most commonly performed gynecological surgical procedure, after cesarean section, in the United States. Nearly 68 percent were performed for conditions such as endometriosis, irregular bleeding, and uterine fibroids. It is expected that the frequency of hysterectomies for non-malignant indications will continue to fall given the development of alternative treatment options.

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.
Heavy menstrual bleeding (HMB), previously known as menorrhagia or hematomunia, is a menstrual period with excessively heavy flow. It is a type of abnormal uterine bleeding (AUB).
Abnormal uterine bleeding (AUB), also known as (AVB) or as atypical vaginal bleeding, is vaginal bleeding from the uterus that is abnormally frequent, lasts excessively long, is heavier than normal, or is irregular. The term dysfunctional uterine bleeding was used when no underlying cause was present. Vaginal bleeding during pregnancy is excluded. Iron deficiency anemia may occur and quality of life may be negatively affected.
Embolization refers to the passage and lodging of an embolus within the bloodstream. It may be of natural origin (pathological), in which sense it is also called embolism, for example a pulmonary embolism; or it may be artificially induced (therapeutic), as a hemostatic treatment for bleeding or as a treatment for some types of cancer by deliberately blocking blood vessels to starve the tumor cells.

Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.

Adenomyosis is a medical condition characterized by the growth of cells that proliferate on the inside of the uterus (endometrium) atypically located among the cells of the uterine wall (myometrium), as a result, thickening of the uterus occurs. As well as being misplaced in patients with this condition, endometrial tissue is completely functional. The tissue thickens, sheds and bleeds during every menstrual cycle.

Vaginal bleeding is any expulsion of blood from the vagina. This bleeding may originate from the uterus, vaginal wall, or cervix. Generally, it is either part of a normal menstrual cycle or is caused by hormonal or other problems of the reproductive system, such as abnormal uterine bleeding.

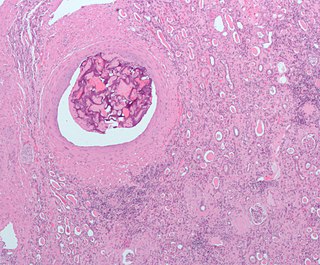
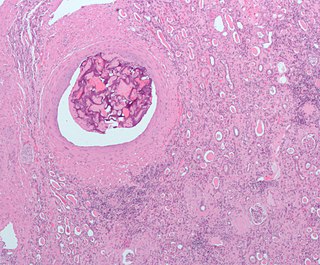
Uterine fibroids, also known as uterine leiomyomas or fibroids, are benign smooth muscle tumors of the uterus. Most women with fibroids have no symptoms while others may have painful or heavy periods. If large enough, they may push on the bladder, causing a frequent need to urinate. They may also cause pain during penetrative sex or lower back pain. A woman can have one uterine fibroid or many. Occasionally, fibroids may make it difficult to become pregnant, although this is uncommon.

Myomectomy, sometimes also called fibroidectomy, refers to the surgical removal of uterine leiomyomas, also known as fibroids. In contrast to a hysterectomy, the uterus remains preserved and the woman retains her reproductive potential. It still may impact hormonal regulation and the menstrual cycle.
Adenomyoma is a tumor (-oma) including components derived from glands (adeno-) and muscle (-my-). It is a type of complex and mixed tumor, and several variants have been described in the medical literature. Uterine adenomyoma, the localized form of uterine adenomyosis, is a tumor composed of endometrial gland tissue and smooth muscle in the myometrium. Adenomyomas containing endometrial glands are also found outside of the uterus, most commonly on the uterine adnexa but can also develop at distant sites outside of the pelvis. Gallbladder adenomyoma, the localized form of adenomyomatosis, is a polypoid tumor in the gallbladder composed of hyperplastic mucosal epithelium and muscularis propria.

Placenta accreta occurs when all or part of the placenta attaches abnormally to the myometrium. Three grades of abnormal placental attachment are defined according to the depth of attachment and invasion into the muscular layers of the uterus:
- Accreta – chorionic villi attached to the myometrium, rather than being restricted within the decidua basalis.
- Increta – chorionic villi invaded into the myometrium.
- Percreta – chorionic villi invaded through the perimetrium.

The uterine artery is an artery that supplies blood to the uterus in females.

Uterine atony is the failure of the uterus to contract adequately following delivery. Contraction of the uterine muscles during labor compresses the blood vessels and slows flow, which helps prevent hemorrhage and facilitates coagulation. Therefore, a lack of uterine muscle contraction can lead to an acute hemorrhage, as the vasculature is not being sufficiently compressed. Uterine atony is the most common cause of postpartum hemorrhage, which is an emergency and potential cause of fatality. Across the globe, postpartum hemorrhage is among the top five causes of maternal death. Recognition of the warning signs of uterine atony in the setting of extensive postpartum bleeding should initiate interventions aimed at regaining stable uterine contraction.

Postpartum bleeding or postpartum hemorrhage (PPH) is often defined as the loss of more than 500 ml or 1,000 ml of blood following childbirth. Some have added the requirement that there also be signs or symptoms of low blood volume for the condition to exist. Signs and symptoms may initially include: an increased heart rate, feeling faint upon standing, and an increased breathing rate. As more blood is lost, the patient may feel cold, blood pressure may drop, and they may become restless or unconscious. The condition can occur up to six weeks following delivery.
Reproductive surgery is surgery in the field of reproductive medicine. It can be used for contraception, e.g. in vasectomy, wherein the vasa deferentia of a male are severed, but is also used plentifully in assisted reproductive technology. Reproductive surgery is generally divided into three categories: surgery for infertility, in vitro fertilization, and fertility preservation.

An interstitial pregnancy is a uterine but ectopic pregnancy; the pregnancy is located outside the uterine cavity in that part of the fallopian tube that penetrates the muscular layer of the uterus. The term cornual pregnancy is sometimes used as a synonym, but remains ambiguous as it is also applied to indicate the presence of a pregnancy located within the cavity in one of the two upper "horns" of a bicornuate uterus. Interstitial pregnancies have a higher mortality than ectopics in general.
Interventional oncology is a subspecialty field of interventional radiology that deals with the diagnosis and treatment of cancer and cancer-related problems using targeted minimally invasive procedures performed under image guidance. Interventional oncology has developed to a separate pillar of modern oncology and it employs X-ray, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) to help guide miniaturized instruments to allow targeted and precise treatment of solid tumours located in various organs of the human body, including but not limited to the liver, kidneys, lungs, and bones. Interventional oncology treatments are routinely carried out by interventional radiologists in appropriate settings and facilities.

Prostatic artery embolization is a non-surgical technique for treatment of benign prostatic hypertrophy (BPH).
Anna-Maria Belli, MD, FCIRSE is a British interventional radiologist known for her work in vascular interventional radiology and for holding leadership positions in interventional radiology societies in Britain and Europe.