History
Lateral Pontine Syndrome was first described in France by French neurologists Pierre Marie (1853-1940), Charles Foix (1882-1927), and Théophile Alajouanine (1890-1980) in 1922. They were the first to identify and describe the symptoms and causes of this syndrome.
In their original description, Pierre Marie, Charles Foix, and Théophile Alajouanine reported findings from autopsies that showed spinal cord necrosis and multiple tortuous and thickened blood vessels on the surface of the spinal cord. This condition was later called necrotizing myelopathy [3] .
They emphasized that in their two cases, no thrombosis was present. They considered the vascular component of the entity they reported to be a wall thickening, without luminal narrowing or obliteration of the cord vessels (arteries as well as veins). They addressed, and ruled out, the possibility of vascular malformations. [4]
These findings significantly contributed to our understanding of this syndrome

An arteriovenous malformation (AVM) is an abnormal connection between arteries and veins, bypassing the capillary system. Usually congenital, this vascular anomaly is widely known because of its occurrence in the central nervous system, but can appear anywhere in the body. The symptoms of AVMs can range from none at all to intense pain or bleeding, and they can lead to other serious medical problems.

Central pontine myelinolysis is a neurological condition involving severe damage to the myelin sheath of nerve cells in the pons. It is predominately iatrogenic (treatment-induced), and is characterized by acute paralysis, dysphagia, dysarthria, and other neurological symptoms.

Foix–Alajouanine syndrome, also called subacute ascending necrotizing myelitis, is a disease caused by an arteriovenous malformation of the spinal cord. In particular, most cases involve dural arteriovenous malformations that present in the lower thoracic or lumbar spinal cord. The condition is named after Charles Foix and Théophile Alajouanine who first described the condition in 1926.

Locked-in syndrome (LIS), also known as pseudocoma, is a condition in which a patient is aware but cannot move or communicate verbally due to complete paralysis of nearly all voluntary muscles in the body except for vertical eye movements and blinking. The individual is conscious and sufficiently intact cognitively to be able to communicate with eye movements. Electroencephalography results are normal in locked-in syndrome. Total locked-in syndrome, or completely locked-in state (CLIS), is a version of locked-in syndrome wherein the eyes are paralyzed as well. Fred Plum and Jerome B. Posner coined the term for this disorder in 1966.

The brainstem is the stalk-like part of the brain that interconnects the cerebrum and diencephalon with the spinal cord. In the human brain, the brainstem is composed of the midbrain, the pons, and the medulla oblongata. The midbrain is continuous with the thalamus of the diencephalon through the tentorial notch.

The internal capsule is a white matter structure situated in the inferomedial part of each cerebral hemisphere of the brain. It carries information past the basal ganglia, separating the caudate nucleus and the thalamus from the putamen and the globus pallidus. The internal capsule contains both ascending and descending axons, going to and coming from the cerebral cortex. It also separates the caudate nucleus and the putamen in the dorsal striatum, a brain region involved in motor and reward pathways.
Lateral medullary syndrome is a neurological disorder causing a range of symptoms due to ischemia in the lateral part of the medulla oblongata in the brainstem. The ischemia is a result of a blockage most commonly in the vertebral artery or the posterior inferior cerebellar artery. Lateral medullary syndrome is also called Wallenberg's syndrome, posterior inferior cerebellar artery (PICA) syndrome and vertebral artery syndrome.
Medial medullary syndrome, also known as inferior alternating syndrome, hypoglossal alternating hemiplegia, lower alternating hemiplegia, or Dejerine syndrome, is a type of alternating hemiplegia characterized by a set of clinical features resulting from occlusion of the anterior spinal artery. This results in the infarction of medial part of the medulla oblongata.

Brain herniation is a potentially deadly side effect of very high pressure within the skull that occurs when a part of the brain is squeezed across structures within the skull. The brain can shift across such structures as the falx cerebri, the tentorium cerebelli, and even through the foramen magnum. Herniation can be caused by a number of factors that cause a mass effect and increase intracranial pressure (ICP): these include traumatic brain injury, intracranial hemorrhage, or brain tumor.
Vertebrobasilar insufficiency (VBI) describes a temporary set of symptoms due to decreased blood flow (ischemia) in the posterior circulation of the brain. The posterior circulation supplies the medulla, pons, midbrain, cerebellum and supplies the posterior cerebellar artery to the thalamus and occipital cortex. As a result, symptoms vary widely depending which brain region is predominantly affected.

The anterior inferior cerebellar artery (AICA) is one of three pairs of arteries that supplies blood to the cerebellum.

The central canal is the cerebrospinal fluid-filled space that runs through the spinal cord. The central canal lies below and is connected to the ventricular system of the brain, from which it receives cerebrospinal fluid, and shares the same ependymal lining. The central canal helps to transport nutrients to the spinal cord as well as protect it by cushioning the impact of a force when the spine is affected.

The basilar part of pons, also known as basis pontis, is the ventral part of the pons; the dorsal part is known as the pontine tegmentum.
Conjugate gaze palsies are neurological disorders affecting the ability to move both eyes in the same direction. These palsies can affect gaze in a horizontal, upward, or downward direction. These entities overlap with ophthalmoparesis and ophthalmoplegia.

Posterior spinal artery syndrome(PSAS), also known as posterior spinal cord syndrome, is a type of incomplete spinal cord injury. PSAS is the least commonly occurring of the six clinical spinal cord injury syndromes, with an incidence rate of less than 1%.
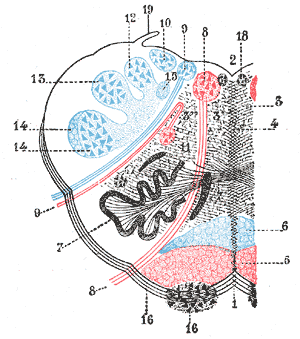
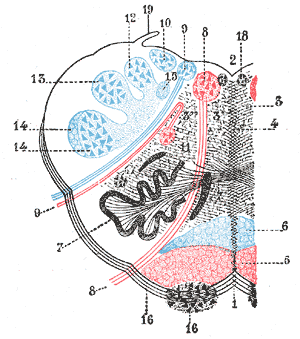
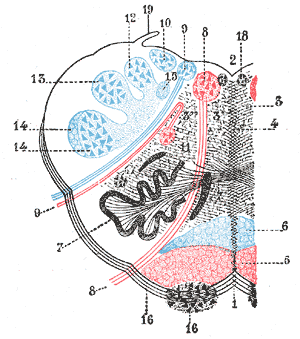
Vascular myelopathy refers to an abnormality of the spinal cord in regard to its blood supply. The blood supply is complicated and supplied by two major vessel groups: the posterior spinal arteries and the anterior spinal arteries—of which the Artery of Adamkiewicz is the largest. Both the posterior and anterior spinal arteries run the entire length of the spinal cord and receive anastomotic (conjoined) vessels in many places. The anterior spinal artery has a less efficient supply of blood and is therefore more susceptible to vascular disease. Whilst atherosclerosis of spinal arteries is rare, necrosis in the anterior artery can be caused by disease in vessels originating from the segmental arteries such as atheroma or aortic dissection.
A brainstem stroke syndrome falls under the broader category of stroke syndromes, or specific symptoms caused by vascular injury to an area of brain. As the brainstem contains numerous cranial nuclei and white matter tracts, a stroke in this area can have a number of unique symptoms depending on the particular blood vessel that was injured and the group of cranial nerves and tracts that are no longer perfused. Symptoms of a brainstem stroke frequently include sudden vertigo and ataxia, with or without weakness. Brainstem stroke can also cause diplopia, slurred speech and decreased level of consciousness. A more serious outcome is locked-in syndrome.

Cervicocranial syndrome or is a neurological illness. It is a combination of symptoms that are caused by an abnormality in the neck. The bones of the neck that are affected are cervical vertebrae (C1-C7). This syndrome can be identified by confirming cervical bone shifts, collapsed cervical bones or misalignment of the cervical bone leading to improper functioning of cervical spinal nerves. Cervicocranial syndrome is either congenital or acquired. Some examples of diseases that could result in cervicocranial syndrome are Chiari disease, Klippel-Feil malformation osteoarthritis, and trauma. Treatment options include neck braces, pain medication and surgery. The quality of life for individuals suffering from CCJ syndrome can improve through surgery.

This glossary of medical terms is a list of definitions about medicine, its sub-disciplines, and related fields.

Mueller–Weiss syndrome, also known as Mueller–Weiss disease, is a rare idiopathic degenerative disease of the adult navicular bone characterized by progressive collapse and fragmentation, leading to mid- and hindfoot pain and deformity. It is most commonly seen in females, ages 40–60. Characteristic imaging shows lateral navicular collapse. This disease had been historically considered to be a form of adult onset osteonecrosis, with blood flow cutoff to the navicular.