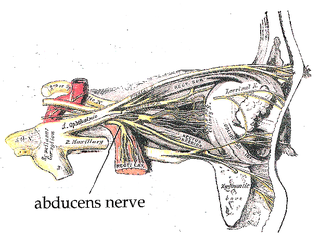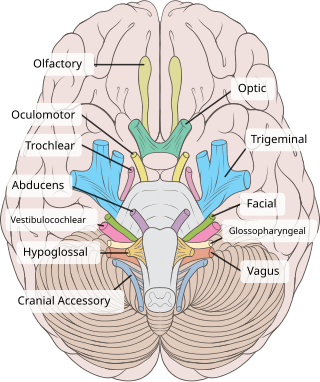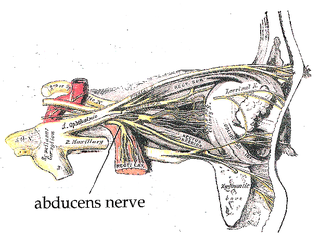
The abducens nerve or abducent nerve, also known as the sixth cranial nerve, cranial nerve VI, or simply CN VI, is a cranial nerve in humans and various other animals that controls the movement of the lateral rectus muscle, one of the extraocular muscles responsible for outward gaze. It is a somatic efferent nerve.
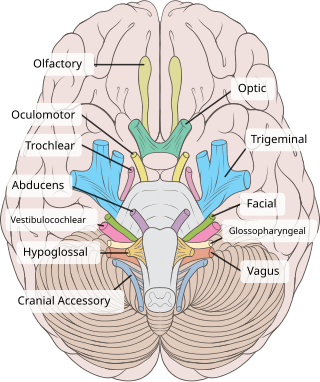
The trochlear nerve, also known as the fourth cranial nerve, cranial nerve IV, or CN IV, is a cranial nerve that innervates a single muscle - the superior oblique muscle of the eye. Unlike most other cranial nerves, the trochlear nerve is exclusively a motor nerve.

The vestibulo-ocular reflex (VOR) is a reflex acting to stabilize gaze during head movement, with eye movement due to activation of the vestibular system. The reflex acts to stabilize images on the retinas of the eye during head movement. Gaze is held steadily on a location by producing eye movements in the direction opposite that of head movement. For example, when the head moves to the right, the eyes move to the left, meaning the image a person sees stays the same even though the head has turned. Since slight head movement is present all the time, VOR is necessary for stabilizing vision: people with an impaired reflex find it difficult to read using print, because the eyes do not stabilise during small head tremors, and also because damage to reflex can cause nystagmus.
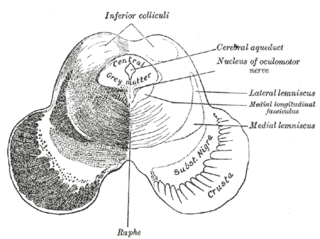
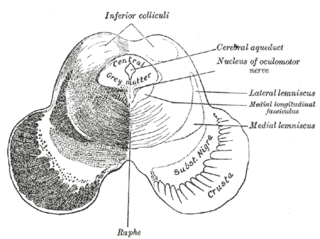
The medial longitudinal fasciculus (MLF) is an area of crossed over tracts, on each side of the brainstem. These bundles of axons are situated near the midline of the brainstem. They are made up of both ascending and descending fibers that arise from a number of sources and terminate in different areas, including the superior colliculus, the vestibular nuclei, and the cerebellum. It contains the interstitial nucleus of Cajal, responsible for oculomotor control, head posture, and vertical eye movement.

The abducens nucleus is the originating nucleus from which the abducens nerve (VI) emerges—a cranial nerve nucleus. This nucleus is located beneath the fourth ventricle in the caudal portion of the pons, medial to the sulcus limitans.

Ophthalmoparesis refers to weakness (-paresis) or paralysis (-plegia) of one or more extraocular muscles which are responsible for eye movements. It is a physical finding in certain neurologic, ophthalmologic, and endocrine disease.

Parinaud's syndrome is an inability to move the eyes up and down. It is caused by compression of the vertical gaze center at the rostral interstitial nucleus of medial longitudinal fasciculus (riMLF). The eyes lose the ability to move upward and down.

The flocculus is a small lobe of the cerebellum at the posterior border of the middle cerebellar peduncle anterior to the biventer lobule. Like other parts of the cerebellum, the flocculus is involved in motor control. It is an essential part of the vestibulo-ocular reflex, and aids in the learning of basic motor skills in the brain.
Opsoclonus refers to uncontrolled, irregular, and nonrhythmic eye movement. Opsoclonus consists of rapid, involuntary, multivectorial, unpredictable, conjugate fast eye movements without inter-saccadic intervals. It is also referred to as saccadomania or reflexive saccade. The movements of opsoclonus may have a very small amplitude, appearing as tiny deviations from primary position.

Sixth nerve palsy, or abducens nerve palsy, is a disorder associated with dysfunction of cranial nerve VI, which is responsible for causing contraction of the lateral rectus muscle to abduct the eye. The inability of an eye to turn outward, results in a convergent strabismus or esotropia of which the primary symptom is diplopia in which the two images appear side-by-side. Thus, the diplopia is horizontal and worse in the distance. Diplopia is also increased on looking to the affected side and is partly caused by overaction of the medial rectus on the unaffected side as it tries to provide the extra innervation to the affected lateral rectus. These two muscles are synergists or "yoke muscles" as both attempt to move the eye over to the left or right. The condition is commonly unilateral but can also occur bilaterally.
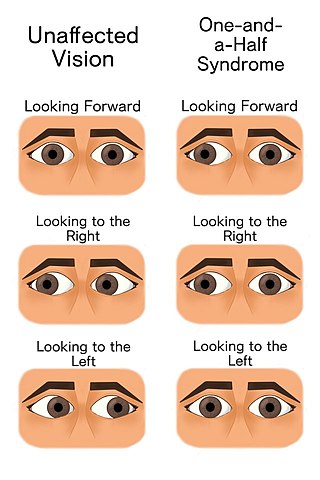
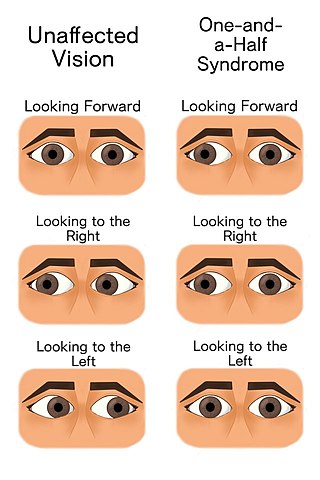
The one and a half syndrome is a rare weakness in eye movement affecting both eyes, in which one cannot move laterally at all, and the other can move only in outward direction. More formally, it is characterized by "a conjugate horizontal gaze palsy in one direction and an internuclear ophthalmoplegia in the other". Nystagmus is also present when the eye on the opposite side of the lesion is abducted. Convergence is classically spared as cranial nerve III and its nucleus is spared bilaterally.

The paramedian pontine reticular formation, also known as PPRF or paraabducens nucleus, is part of the pontine reticular formation, a brain region without clearly defined borders in the center of the pons. It is involved in the coordination of eye movements, particularly horizontal gaze and saccades.

The facial motor nucleus is a collection of neurons in the brainstem that belong to the facial nerve. These lower motor neurons innervate the muscles of facial expression and the stapedius.

Foville's syndrome is caused by the blockage of the perforating branches of the basilar artery in the region of the brainstem known as the pons. It is most frequently caused by lesions such as vascular disease and tumors involving the dorsal pons.

Multiple sclerosis can cause a variety of symptoms: changes in sensation (hypoesthesia), muscle weakness, abnormal muscle spasms, or difficulty moving; difficulties with coordination and balance; problems in speech (dysarthria) or swallowing (dysphagia), visual problems, fatigue and acute or chronic pain syndromes, bladder and bowel difficulties, cognitive impairment, or emotional symptomatology. The main clinical measure in progression of the disability and severity of the symptoms is the Expanded Disability Status Scale or EDSS.
Conjugate gaze palsies are neurological disorders affecting the ability to move both eyes in the same direction. These palsies can affect gaze in a horizontal, upward, or downward direction. These entities overlap with ophthalmoparesis and ophthalmoplegia.

Nystagmus is a condition of involuntary eye movement, sometimes informally called "dancing eyes". People can be born with it but more commonly acquire it in infancy or later in life. In many cases it may result in reduced or limited vision.
Conjugate eye movement refers to motor coordination of the eyes that allows for bilateral fixation on a single object. A conjugate eye movement is a movement of both eyes in the same direction to maintain binocular gaze. This is in contrast to vergence eye movement, where binocular gaze is maintained by moving eyes in opposite directions, such as going “cross eyed” to view an object moving towards the face. Conjugate eye movements can be in any direction, and can accompany both saccadic eye movements and smooth pursuit eye movements.
Alternating hemiplegia is a form of hemiplegia that has an ipsilateral cranial nerve palsies and contralateral hemiplegia or hemiparesis of extremities of the body. The disorder is characterized by recurrent episodes of paralysis on one side of the body. There are multiple forms of alternating hemiplegia, Weber's syndrome, middle alternating hemiplegia, and inferior alternating hemiplegia. This type of syndrome can result from a unilateral lesion in the brainstem affecting both upper motor neurons and lower motor neurons. The muscles that would receive signals from these damaged upper motor neurons result in spastic paralysis. With a lesion in the brainstem, this affects the majority of limb and trunk muscles on the contralateral side due to the upper motor neurons decussation after the brainstem. The cranial nerves and cranial nerve nuclei are also located in the brainstem making them susceptible to damage from a brainstem lesion. Cranial nerves III (Oculomotor), VI (Abducens), and XII (Hypoglossal) are most often associated with this syndrome given their close proximity with the pyramidal tract, the location which upper motor neurons are in on their way to the spinal cord. Damages to these structures produce the ipsilateral presentation of paralysis or palsy due to the lack of cranial nerve decussation before innervating their target muscles. The paralysis may be brief or it may last for several days, many times the episodes will resolve after sleep. Some common symptoms of alternating hemiplegia are mental impairment, gait and balance difficulties, excessive sweating and changes in body temperature.
In neuroanatomy, corticomesencephalic tract is a descending nerve tract that originates in the frontal eye field and terminate in the midbrain. Its fibers mediate conjugate eye movement.