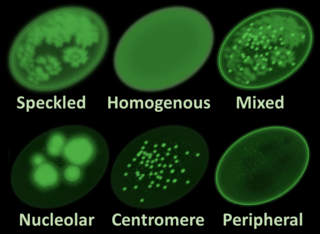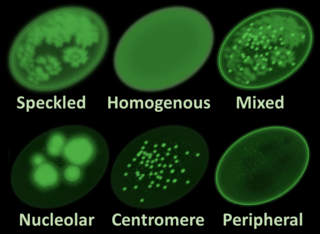
Antinuclear antibodies are autoantibodies that bind to contents of the cell nucleus. In normal individuals, the immune system produces antibodies to foreign proteins (antigens) but not to human proteins (autoantigens). In some cases, antibodies to human antigens are produced.

Kikuchi disease was described in 1972 in Japan. It is also known as histiocytic necrotizing lymphadenitis, Kikuchi necrotizing lymphadenitis, phagocytic necrotizing lymphadenitis, subacute necrotizing lymphadenitis, and necrotizing lymphadenitis. Kikuchi disease occurs sporadically in people with no family history of the condition.

Lupus nephritis is an inflammation of the kidneys caused by systemic lupus erythematosus (SLE), an autoimmune disease. It is a type of glomerulonephritis in which the glomeruli become inflamed. Since it is a result of SLE, this type of glomerulonephritis is said to be secondary, and has a different pattern and outcome from conditions with a primary cause originating in the kidney. The diagnosis of lupus nephritis depends on blood tests, urinalysis, X-rays, ultrasound scans of the kidneys, and a kidney biopsy. On urinalysis, a nephritic picture is found and red blood cell casts, red blood cells and proteinuria is found.
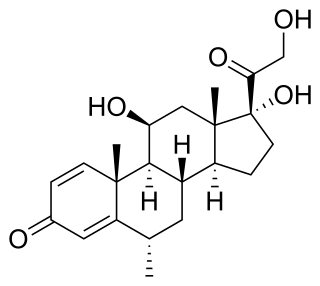
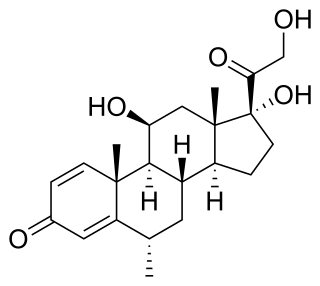
Methylprednisolone is a synthetic glucocorticoid, primarily prescribed for its anti-inflammatory and immunosuppressive effects. It is either used at low doses for chronic illnesses or used concomitantly at high doses during acute flares. Methylprednisolone and its derivatives can be administered orally or parenterally.
An autoantibody is an antibody produced by the immune system that is directed against one or more of the individual's own proteins. Many autoimmune diseases are associated with such antibodies.
A connective tissue disease is a disease which involves damage to, or destruction of, any type of connective tissue in the body. Depending on the specific disease, the affected tissue(s) may be a single specific type, a group of several related tissues, or a wide variety of unrelated types of connective tissue. Some of the most common connective tissue diseases involve injury to collagen and elastin as a result of inflammation. Many connective tissue diseases are strongly connected to autoimmune disease processes.
Mixed connective tissue disease, commonly abbreviated as MCTD, is an autoimmune disease characterized by the presence of elevated blood levels of a specific autoantibody, now called anti-U1 ribonucleoprotein (RNP), together with a mix of symptoms of systemic lupus erythematosus (SLE), scleroderma, and polymyositis. The idea behind the "mixed" disease is that this specific autoantibody is also present in other autoimmune diseases such as systemic lupus erythematosus, polymyositis, scleroderma, etc. MCTD was characterized as an individual disease in 1972 by Sharp et al., and the term was introduced by Leroy in 1980.

Drug-induced lupus erythematosus is an autoimmune disorder caused by chronic use of certain drugs. These drugs cause an autoimmune response producing symptoms similar to those of systemic lupus erythematosus (SLE). There are 38 known medications to cause DIL but there are three that report the highest number of cases: hydralazine, procainamide, and quinidine. While the criteria for diagnosing DIL has not been thoroughly established, symptoms of DIL typically present as muscle pain and joint pain. Generally, the symptoms recede after discontinuing use of the drugs.

HLA-DR4 (DR4) is an HLA-DR serotype that recognizes the DRB1*04 gene products. The DR4 serogroup is large and has a number of moderate frequency alleles spread over large regions of the world.

Discoid lupus erythematosus is the most common type of chronic cutaneous lupus (CCLE), an autoimmune skin condition on the lupus erythematosus spectrum of illnesses. It presents with red, painful, inflamed and coin-shaped patches of skin with a scaly and crusty appearance, most often on the scalp, cheeks, and ears. Hair loss may occur if the lesions are on the scalp. The lesions can then develop severe scarring, and the centre areas may appear lighter in color with a rim darker than the normal skin. These lesions can last for years without treatment.

An autoimmune disease is a condition that results from an anomalous response of the adaptive immune system, wherein it mistakenly targets and attacks healthy, functioning parts of the body as if they were foreign organisms. It is estimated that there are more than 80 recognized autoimmune diseases, with recent scientific evidence suggesting the existence of potentially more than 100 distinct conditions. Nearly any body part can be involved.

Anti-double stranded DNA (Anti-dsDNA) antibodies are a group of anti-nuclear antibodies (ANA) the target antigen of which is double stranded DNA. Blood tests such as enzyme-linked immunosorbent assay (ELISA) and immunofluorescence are routinely performed to detect anti-dsDNA antibodies in diagnostic laboratories. They are highly diagnostic of systemic lupus erythematosus (SLE) and are implicated in the pathogenesis of lupus nephritis.
Tumid lupus erythematosus is a rare, but distinctive entity in which patients present with edematous erythematous plaques, usually on the trunk.
Subacute cutaneous lupus erythematosus is a clinically distinct subset of cases of lupus erythematosus that is most often present in white women aged 15 to 40, consisting of skin lesions that are scaly and evolve as poly-cyclic annular lesions or plaques similar to those of plaque psoriasis.

Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face. Often there are periods of illness, called flares, and periods of remission during which there are few symptoms.
Diffuse proliferative glomerulonephritis (DPGN) is a type of glomerulonephritis that is the most serious form of renal lesions in SLE and is also the most common, occurring in 35% to 60% of patients. In absence of SLE, DPGN pathology looks more like Membranoproliferative glomerulonephritis
Acute cutaneous lupus erythematosus is a cutaneous condition characterized by a bilateral malar rash and lesions that tend to be transient, and that follow sun exposure. The acute form is distinct from chronic and subacute cutaneous lupus erythematosus, which may have different types of skin lesions. Cutaneous lupus erythematosus is associated with both lupus erythematosus-specific lesions and cutaneous manifestations that are not specific to lupus erythematosus, such as oral ulcers and urticaria. Because of the diagnostic criteria used to diagnose systemic lupus erythematosus, a patient with only cutaneous manifestations may be diagnosed with the systemic form of the disease.

Anti-SSA autoantibodies are a type of anti-nuclear autoantibodies that are associated with many autoimmune diseases, such as systemic lupus erythematosus (SLE), SS/SLE overlap syndrome, subacute cutaneous lupus erythematosus (SCLE), neonatal lupus and primary biliary cirrhosis. They are often present in Sjögren's syndrome (SS). Additionally, Anti-Ro/SSA can be found in other autoimmune diseases such as systemic sclerosis (SSc), polymyositis/dermatomyositis (PM/DM), rheumatoid arthritis (RA), and mixed connective tissue disease (MCTD), and are also associated with heart arrhythmia.

Lupus vasculitis is one of the secondary vasculitides that occurs in approximately 50% of patients with systemic lupus erythematosus (SLE).
Neuropsychiatric systemic lupus erythematosus or NPSLE refers to the neurological and psychiatric manifestations of systemic lupus erythematosus. SLE is a disease in which the immune system attacks the body's own cells and tissues. It can affect various organs or systems of the body. It is estimated that over half of people with SLE have neuropsychiatric involvement.