Related Research Articles

Riboflavin, also known as vitamin B2, is a vitamin found in food and sold as a dietary supplement. It is essential to the formation of two major coenzymes, flavin mononucleotide and flavin adenine dinucleotide. These coenzymes are involved in energy metabolism, cellular respiration, and antibody production, as well as normal growth and development. The coenzymes are also required for the metabolism of niacin, vitamin B6, and folate. Riboflavin is prescribed to treat corneal thinning, and taken orally, may reduce the incidence of migraine headaches in adults.

Vitamin B6 is one of the B vitamins, and thus an essential nutrient. The term refers to a group of six chemically similar compounds, i.e., "vitamers", which can be interconverted in biological systems. Its active form, pyridoxal 5′-phosphate, serves as a coenzyme in more than 140 enzyme reactions in amino acid, glucose, and lipid metabolism.
Vitamin deficiency is the condition of a long-term lack of a vitamin. When caused by not enough vitamin intake it is classified as a primary deficiency, whereas when due to an underlying disorder such as malabsorption it is called a secondary deficiency. An underlying disorder can have 2 main causes:
Paresthesia is an abnormal sensation of the skin with no apparent physical cause. Paresthesia may be transient or chronic, and may have many possible underlying causes. Paresthesias are usually painless and can occur anywhere on the body, but most commonly occur in the arms and legs.
B vitamins are a class of water-soluble vitamins that play important roles in cell metabolism and synthesis of red blood cells. They are a chemically diverse class of compounds; some contain sulfur and B12 contains cobalt. Dietary supplements containing all eight are referred to as a vitamin B complex. Individual B vitamins are referred to by B-number or by chemical name, such as B1 for thiamine, B2 for riboflavin, and B3 for niacin, while some are more commonly recognized by name than by number, such as pantothenic acid (B5), biotin (B7), and folate (B9).
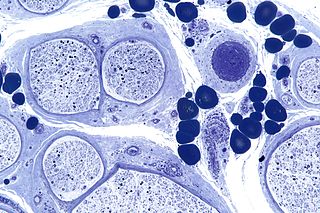
Peripheral neuropathy, often shortened to neuropathy, refers to damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerves are affected. Neuropathies affecting motor, sensory, or autonomic nerves result in different symptoms. More than one type of nerve may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.

Hypervitaminosis is a condition of abnormally high storage levels of vitamins, which can lead to various symptoms as over excitement, irritability, or even toxicity. Specific medical names of the different conditions are derived from the given vitamin involved: an excess of vitamin A, for example, is called hypervitaminosis A. Hypervitaminoses are primarily caused by fat-soluble vitamins, as these are stored by the body for longer than the water-soluble vitamins.

Pyridoxine, is a form of vitamin B6 found commonly in food and used as a dietary supplement. As a supplement it is used to treat and prevent pyridoxine deficiency, sideroblastic anaemia, pyridoxine-dependent epilepsy, certain metabolic disorders, side effects or complications of isoniazid use, and certain types of mushroom poisoning. It is used by mouth or by injection.

Alcoholic polyneuropathy is a neurological disorder in which peripheral nerves throughout the body malfunction simultaneously. It is defined by axonal degeneration in neurons of both the sensory and motor systems and initially occurs at the distal ends of the longest axons in the body. This nerve damage causes an individual to experience pain and motor weakness, first in the feet and hands and then progressing centrally. Alcoholic polyneuropathy is caused primarily by chronic alcoholism; however, vitamin deficiencies are also known to contribute to its development. This disease typically occurs in chronic alcoholics who have some sort of nutritional deficiency. Treatment may involve nutritional supplementation, pain management, and abstaining from alcohol.

Neuritis, from the Greek νεῦρον), is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.

Hypervitaminosis A refers to the toxic effects of ingesting too much preformed vitamin A. Symptoms arise as a result of altered bone metabolism and altered metabolism of other fat-soluble vitamins. Hypervitaminosis A is believed to have occurred in early humans, and the problem has persisted throughout human history. Toxicity results from ingesting too much preformed vitamin A from foods, supplements, or prescription medications and can be prevented by ingesting no more than the recommended daily amount.
Megavitamin therapy is the use of large doses of vitamins, often many times greater than the recommended dietary allowance (RDA) in the attempt to prevent or treat diseases. Megavitamin therapy is typically used in alternative medicine by practitioners who call their approach orthomolecular medicine. Vitamins are useful in preventing and treating illnesses specifically associated with dietary vitamin shortfalls, but the conclusions of medical research are that the broad claims of disease treatment by advocates of megavitamin therapy are unsubstantiated by the available evidence. It is generally accepted that doses of any vitamin greatly in excess of nutritional requirements will result either in toxicity or in the excess simply being metabolised; thus evidence in favour of vitamin supplementation supports only doses in the normal range. Critics have described some aspects of orthomolecular medicine as food faddism or even quackery. Research on nutrient supplementation in general suggests that some nutritional supplements might be beneficial, and that others might be harmful; several specific nutritional therapies are associated with an increased likelihood of the condition they are meant to prevent.
Toxic and nutritional optic neuropathy is a group of medical disorders defined by visual impairment due to optic nerve damage secondary to a toxic substance and/or nutritional deficiency. The causes of these disorders are various, but they are linked by shared signs and symptoms, which this article will describe. In several of these disorders, both toxic and nutritional factors play a role, acting synergistically.

Subacute combined degeneration of spinal cord, also known as myelosis funiculus, or funicular myelosis, also Lichtheim's disease, and Putnam-Dana syndrome, refers to degeneration of the posterior and lateral columns of the spinal cord as a result of vitamin B12 deficiency (most common). It may also occur similarly as result of vitamin E deficiency, and copper deficiency. It is usually associated with pernicious anemia.
Vitamins occur in a variety of related forms known as vitamers. A vitamer of a particular vitamin is one of several related compounds that performs the functions of said vitamin and prevents the symptoms of deficiency of said vitamin.

Pyridoxine-dependent epilepsy (PDE) is a rare genetic disorder characterized by intractable seizures in the prenatal and neonatal period. The disorder was first recognized in the 1950s, with the first description provided by Hunt et al. in 1954. More recently, pathogenic variants within the ALDH7A1 gene have been identified to cause PDE.

Nutritional neuroscience is the scientific discipline that studies the effects various components of the diet such as minerals, vitamins, protein, carbohydrates, fats, dietary supplements, synthetic hormones, and food additives have on neurochemistry, neurobiology, behavior, and cognition.
Sexual anhedonia, also known as pleasure dissociative orgasmic disorder, is a condition in which an individual cannot feel pleasure from an orgasm. It is thought to be a variant of hypoactive sexual desire disorder.
Relatively speaking, the brain consumes an immense amount of energy in comparison to the rest of the body. The mechanisms involved in the transfer of energy from foods to neurons are likely to be fundamental to the control of brain function. Human bodily processes, including the brain, all require both macronutrients, as well as micronutrients.
Mitochondrial optic neuropathies are a heterogenous group of disorders that present with visual disturbances resultant from mitochondrial dysfunction within the anatomy of the Retinal Ganglion Cells (RGC), optic nerve, optic chiasm, and optic tract. These disturbances are multifactorial, their aetiology consisting of metabolic and/or structural damage as a consequence of genetic mutations, environmental stressors, or both. The three most common neuro-ophthalmic abnormalities seen in mitochondrial disorders are bilateral optic neuropathy, ophthalmoplegia with ptosis, and pigmentary retinopathy.
References
- 1 2 Bell, Daniel J. "Vitamin B6 excess". Radiopaedia. Archived from the original on 2019-10-24. Retrieved 2019-12-01.
Vitamin B6 excess (hypervitaminosis B6) is caused by excessive consumption of supplemental pyridoxine, which is used as a therapeutic agent for several conditions.
- 1 2 "Hypervitaminosis B6 (Concept Id: C0238176) - MedGen - NCBI". MedGen. National Center for Biotechnology Information (NCBI). Archived from the original on 2019-11-05. Retrieved 2019-12-02.
- 1 2 3 4 5 6 7 8 9 Koontz, Daniel W; Maddux, Brian; Katirji, Bashar (2004). "Evaluation of a Patient Presenting With Rapidly Progressive Sensory Ataxia". Journal of Clinical Neuromuscular Disease. 6 (1): 40–47. doi:10.1097/01.cnd.0000133065.28161.00. ISSN 1522-0443. PMID 19078751. S2CID 26316070.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Lheureux, P.; Penaloza, A.; Gris, M. (2005). "Pyridoxine in clinical toxicology: A review". European Journal of Emergency Medicine. 12 (2): 78–85. doi:10.1097/00063110-200504000-00007. PMID 15756083. S2CID 39197646.
- 1 2 Silva, C D; D'Cruz, D P (2006). "Pyridoxine toxicity courtesy of your local health food store". Annals of the Rheumatic Diseases. 65 (12): 1666–1667. doi:10.1136/ard.2006.054213. ISSN 0003-4967. PMC 1798481 . PMID 17105856.
Pyridoxine toxicity is a recognised cause of sensory neuropathy. Schaumburg et al described sensory neuropathy after pyridoxine misuse in 1983. It can occur with chronic use of pyridoxine supplementation over several years, and also with acute over-dosage with parenteral pyridoxine.
- 1 2 3 4 James W. Albers; Stanley Berent (15 August 2005). Neurobehavioral Toxicology: Neurological and Neuropsychological Perspectives, Volume II: Peripheral Nervous System. Taylor & Francis. pp. 2–. ISBN 978-1-135-42106-9.
- 1 2 Kennedy, Ashleigh; Schaeffer, Tammi (2016). "Pyridoxine". Critical Care Toxicology. pp. 1–4. doi:10.1007/978-3-319-20790-2_174-1. ISBN 978-3-319-20790-2.
- 1 2 3 London, Zachary; Albers, James W. (2007). "Toxic Neuropathies Associated with Pharmaceutic and Industrial Agents". Neurologic Clinics. 25 (1): 257–276. doi:10.1016/j.ncl.2006.10.001. ISSN 0733-8619. PMID 17324727.
- ↑ Mikalunas, Vida; Fitzgerald, Kathleen; Rubin, Halina; McCarthy, Roberta; Craig, Robert M. (2001). "Abnormal Vitamin Levels in Patients Receiving Home Total Parenteral Nutrition". Journal of Clinical Gastroenterology. 33 (5): 393–396. doi:10.1097/00004836-200111000-00010. ISSN 0192-0790. PMID 11606856. S2CID 12384721.
- 1 2 3 4 5 Donofrio, Peter D. (2005). "Evaluating the Patient With Peripheral Neuropathy" (PDF). Numbness, Tingling, Pain, and Weakness: A Basic Course in Electrodiagnostic Medicine. Monterey, California: AANEM 52nd Annual Scientific Meeting. Archived from the original (PDF) on 2022-03-31. Retrieved 2019-11-16.
- 1 2 3 Rohitha Moudgal; Shahla Hosseini; Patricia Colapietro; Oluwole Awosika (2018-04-25). "Vitamin B6 Toxicity Revisited: A Case of Reversible Pyridoxine-associated Neuropathy and Disequilibrium. (P4.021)". Neurology. 90 (15 Supplement). Archived from the original on 2019-10-20. Retrieved 2019-11-16.
- 1 2 3 4 5 6 7 8 Ahmed, Aiesha; Velazquez-Rodriguez, Yadira; Kaur, Divpreet (2014-04-08). "When Expected Turns Unexpected: A Case of Subacute Progressive Weakness and Paresthesias of the Distal Lower Extremities Following a Brief Diarrheal Episode. (P6.111)". Neurology. 82 (10 Supplement): P6.111. Archived from the original on 2019-09-27. Retrieved 2019-11-26.
- 1 2 3 4 Scott, K.; Zeris, S.; Kothari, M. J. (2008). "Elevated B6 levels and peripheral neuropathies". Electromyography and Clinical Neurophysiology. 48 (5): 219–23. PMID 18754531.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Hammond, N.; Wang, Y.; Dimachkie, M.; Barohn, R. (2013). "Nutritional Neuropathies". Neurologic Clinics. 31 (2): 477–489. doi:10.1016/j.ncl.2013.02.002. PMC 4199287 . PMID 23642720.
- 1 2 3 4 5 6 7 8 9 Bromberg, Mark B. (2000). "Peripheral Neurotoxic Disorders". Neurologic Clinics. 18 (3): 681–694. doi:10.1016/S0733-8619(05)70218-8. ISSN 0733-8619. PMID 10873238.
- 1 2 3 4 Saleh, Firas G.; Seidman, Roberta J. (2003-12-01). "Drug-Induced Myopathy and Neuropathy". Journal of Clinical Neuromuscular Disease. 5 (2): 81–91. doi:10.1097/00131402-200312000-00003. PMID 19078725. S2CID 31440274.
- 1 2 Sène, Damien (2018). "Small fiber neuropathy: Diagnosis, causes, and treatment". Joint Bone Spine. 85 (5): 553–559. doi:10.1016/j.jbspin.2017.11.002. ISSN 1297-319X. PMID 29154979. S2CID 43023310.
- 1 2 3 4 5 Hlubocky, Ales; Smith, Benn E. (2014). "Dorsal Root Ganglion Disorders". Neuromuscular Disorders in Clinical Practice. pp. 467–491. doi:10.1007/978-1-4614-6567-6_23. ISBN 978-1-4614-6566-9.
- 1 2 3 Lacerna, Rhodora A.; Chien, Chloe; Yeh, Shing-Shing (2003). "Paresthesias Developing in an Elderly Patient after Chronic Usage of Nitrofurantoin and Vitamin B6". Journal of the American Geriatrics Society. 51 (12): 1822–1823. doi:10.1046/j.1532-5415.2003.51572_8.x. PMID 14687374. S2CID 26337220.
- 1 2 Donofrio, Peter Daniel (2000). "Electrophysiological Evaluations". Neurologic Clinics. 18 (3): 601–613. doi:10.1016/S0733-8619(05)70213-9. ISSN 0733-8619. PMID 10873233. Archived from the original on 2020-01-17. Retrieved 2019-12-01.
- ↑ Schaeppi, U.; Krinke, G. (1982). "Pyridoxine neuropathy: Correlation of functional tests and neuropathology in beagle dogs treated with large doses of vitamin B6". Agents and Actions. 12 (4): 575–582. doi:10.1007/BF01965944. ISSN 0065-4299. PMID 7180742. S2CID 30742144.
- ↑ de Onis, Mercedes; Zeitlhuber, Julia; Martínez-Costa, Cecilia (2016). "Nutritional disorders in the proposed 11th revision of the International Classification of Diseases: feedback from a survey of stakeholders". Public Health Nutrition. 19 (17): 3135–3141. doi:10.1017/S1368980016001427. ISSN 1368-9800. PMC 5217466 . PMID 27293047.
- 1 2 3 4 5 6 7 8 9 10 Gangsaas, Ingvild (1995). "Dispelling the Myths of Vitamin B6" (PDF). Nutrition Bytes. 1 (1). ISSN 1548-4327. Archived (PDF) from the original on 2019-10-21. Retrieved 2019-11-16.
- 1 2 3 4 Callizot, Noëlle; Poindron, Philippe (2008). "Pyridoxine-Induced Peripheral Neuropathy". New Animal Models of Human Neurological Diseases. Biovalley Monographs. pp. 66–80. doi:10.1159/000117724. ISBN 978-3-8055-8405-0.
....a specific large-fibre neuropathy (with severe loss of proprioceptive function) is encountered clinically after vitamin B6 (pyridoxine).... All subjects showed paraesthesia and numbness as well as ataxia. The clinical examination showed a large sensory deficit with Achilles' reflex loss, associated with Romberg's signs (loss of proprioceptive control in which increased unsteadiness occurs when standing with the eyes closed compared with standing with the eyes open). The electromyographic examination showed a large sensory wave amplitude decrease but no change in the motor conduction.... small fibres were also involved as shown by the decreased SNCV and the altered thermosensitivity detected in the hot plate test. The same signs are observed in humans suffering from pyridoxine-induced neuropathy.
- 1 2 3 4 Wilmshurst, Jo M.; Ouvrier, Robert A.; Ryan, Monique M. (2019). "Peripheral nerve disease secondary to systemic conditions in children". Therapeutic Advances in Neurological Disorders. 12: 175628641986636. doi:10.1177/1756286419866367. PMC 6691669 . PMID 31447934.
- 1 2 3 4 5 6 7 8 "Vitamin B6 — Health Professional Fact Sheet". National Institutes of Health Office Dietary Supplements. U.S. Department of Health and Human Services. Archived from the original on 2019-11-25. Retrieved 2019-12-02.
- 1 2 Stover, Patrick J; Field, Martha S (2015). "Vitamin B-6". Advances in Nutrition. 6 (1): 132–133. doi:10.3945/an.113.005207. ISSN 2161-8313. PMC 4288272 . PMID 25593152.
- 1 2 3 Chawla, Jasvinder; Kvarnberg, David (2014). "Hydrosoluble vitamins". Neurologic Aspects of Systemic Disease Part II. Handbook of Clinical Neurology. Vol. 120. pp. 891–914. doi:10.1016/B978-0-7020-4087-0.00059-0. ISBN 978-0-7020-4087-0. ISSN 0072-9752. PMID 24365359.
- 1 2 Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes and its Panel on Folate, Other B Vitamins, and Choline (1998). "Vitamin B6". Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington (DC): National Academies Press (US). Archived from the original on 2021-02-27. Retrieved 2019-12-02.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ↑ Dieb, Wisam; Boucher, Yves (2017). "Burning Mouth Syndome and Vitamin B6". Pain Medicine. 18 (8): 1593–1594. doi: 10.1093/pm/pnw345 . ISSN 1526-2375. PMID 28371806.
- ↑ Dieb, Wisam; Moreau, Nathan; Rochefort, Juliette; Boucher, Yves (2016). "Role of vitamin B6 in idiopathic burning mouth syndrome: some clinical observations" (PDF). Médecine Buccale Chirurgie Buccale. 23 (2): 77–83. doi: 10.1051/mbcb/2016038 . ISSN 1273-2761. Archived (PDF) from the original on 2018-12-06. Retrieved 2019-11-16.
- ↑ Hani R. Khouzam; Doris Tiu Tan; Tirath S. Gill (9 March 2007). Handbook of Emergency Psychiatry E-Book. Elsevier Health Sciences. pp. 65–. ISBN 978-0-323-07661-6.
- ↑ De Kruijk, J. R.; Notermans, N. C. (2005). "Sensory disturbances caused by multivitamin preparations". Nederlands Tijdschrift voor Geneeskunde. 149 (46): 2541–4. PMID 16320661.
- ↑ Levine, Seymour; Saltzman, Arthur (2004). "Pyridoxine (vitamin B6) neurotoxicity: enhancement by protein-deficient diet". Journal of Applied Toxicology. 24 (6): 497–500. doi:10.1002/jat.1007. ISSN 0260-437X. PMID 15558839. S2CID 8280774.
- ↑ Vrolijk, M. F.; Opperhuizen, A.; Jansen EHJM; Hageman, G. J.; Bast, A.; Haenen GRMM (2017). "The vitamin B6 paradox: Supplementation with high concentrations of pyridoxine leads to decreased vitamin B6 function". Toxicology in Vitro. 44: 206–212. doi:10.1016/j.tiv.2017.07.009. PMID 28716455.
- ↑ Windebank, Anthony J. (1985). "Neurotoxicity of pyridoxine analogs is related to coenzyme structure". Neurochemical Pathology. 3 (3): 159–167. doi:10.1007/BF02834268. ISSN 0734-600X. PMID 4094726.
- ↑ Hadtstein, Felix; Vrolijk, Misha (2021). "Vitamin B-6-Induced Neuropathy: Exploring the Mechanisms of Pyridoxine Toxicity". Advances in Nutrition. 12 (5): 1911–1929. doi: 10.1093/advances/nmab033 . PMC 8483950 . PMID 33912895.
- ↑ Ramos, Rúben J.; Albersen, Monique; Vringer, Esmee; Bosma, Marjolein; Zwakenberg, Susan; Zwartkruis, Fried; Jans, Judith J.M.; Verhoeven-Duif, Nanda M. (2019). "Discovery of pyridoxal reductase activity as part of human vitamin B6 metabolism". Biochimica et Biophysica Acta (BBA) - General Subjects. 1863 (6): 1088–1098. doi: 10.1016/j.bbagen.2019.03.019 . ISSN 0304-4165. PMID 30928491. S2CID 89618004.
- 1 2 3 4 5 Assessment of vitamin B6 intake in relation to tolerable upper intake levels. Opinion of the Panel on Nutrition, Dietetic Products, Novel Food and Allergy of the Norwegian Scientific Committee for Food Safety (PDF). Oslo, Norway. ISBN 978-82-8259-260-4. Archived from the original (PDF) on 2019-11-17. Retrieved 2019-12-07.
Eighty to ninety percent of vitamin B6 in the body is found in muscles and estimated body stores in adults amount to about 170 mg with a half-life of 25-33 days... Intakes of vitamin B6 from the diet alone have not been reported to cause adverse effects... (See: Table 2.2.1-1 for summary of available upper intake levels for vitamin B6.
- ↑ Kennedy, Ashleigh; Schaeffer, Tammi (2016). "Pyridoxine". Critical Care Toxicology. pp. 1–4. doi:10.1007/978-3-319-20790-2_174-1. ISBN 978-3-319-20790-2.
The half-life of pyridoxine is up to 20 days.
- ↑ Reeds, Karen (2019-03-04). Ann Ehrenberger, Kristen; Haushofer, Lisa (eds.). "Vitamin B Complexities". H-Nutrition. Archived from the original on 2021-05-12. Retrieved 2019-11-16.
- ↑ Institute of Medicine (29 September 2006). Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. National Academies Press. pp. 184–. ISBN 978-0-309-15742-1. Archived from the original on 19 March 2024. Retrieved 7 December 2019.
- ↑ "Vitamins and minerals - B vitamins and folic acid - NHS". National Health Service . 3 March 2017. Archived from the original on 2019-10-21. Retrieved 2019-11-01.
- ↑ "Advies van BuRO over vitamine B6 uit voedingssupplementen". Netherlands Food and Consumer Product Safety Authority (in Dutch). 2016-12-16. Archived from the original on 2019-12-07. Retrieved 2019-12-07.
- ↑ "Opinion of the Scientific Committee on Food on the Tolerable Upper Intake Level of Vitamin B6" (PDF). Tolerable upper intake levels for vitamins and minerals. European Food Safety Authority (EFSA). 2006. pp. 29–44. ISBN 978-92-9199-014-6. Archived from the original (PDF) on 2019-04-12.
- ↑ "Overview of Dietary Reference Intakes for Japanese" (PDF). Ministry of Health, Labour and Welfare (Japan). 2015. Archived from the original (PDF) on 2021-08-19. Retrieved 19 August 2021.
- ↑ "Vitamin B6". Nutrient Reference Values for Australia and New Zealand. National Health and Medication Research Council (NHMRC). 2014-03-17. Archived from the original on 2019-03-04. Retrieved 2019-12-02.
- ↑ Ghavanini, A. A.; Kimpinski, K. (2014). "Revisiting the evidence for neuropathy caused by pyridoxine deficiency and excess". Journal of Clinical Neuromuscular Disease. 16 (1): 25–31. doi:10.1097/CND.0000000000000049. PMID 25137514. S2CID 205557831.
- ↑ Bender, David A. (1997). "Vitamin B6". Nutrition & Food Science. 97 (4): 128–133. doi:10.1108/00346659710179642. ISSN 0034-6659.
- 1 2 Adverse Drug Reactions Advisory Committee (ADRAC) and the Office of Medicine Safety Monitoring (OMSM) of the TGA. (2008-08-01). "High-dose vitamin B6 may cause peripheral neuropathy". Australian Adverse Drug Reactions Bulletin. 27 (4). Archived from the original on 2017-09-23.
- ↑ Vrolijk, Misha F; Hageman, Geja J; van de Koppel, Sonja; van Hunsel, Florence; Bast, Aalt (2020). "Inter-individual differences in pharmacokinetics of vitamin B6: A possible explanation of different sensitivity to its neuropathic effects". PharmaNutrition. 12: 100188. doi: 10.1016/j.phanu.2020.100188 . ISSN 2213-4344. S2CID 216338587.
- ↑ Van Hunsel, Florence; Van De Koppel, Sonja; Van Puijenbroek, Eugène; Kant, Agnes (2018). "Vitamin B6 in Health Supplements and Neuropathy: Case Series Assessment of Spontaneously Reported Cases" (PDF). Drug Safety. 41 (9): 859–869. doi:10.1007/s40264-018-0664-0. PMID 29737502. S2CID 13685351. Archived (PDF) from the original on 2022-04-08. Retrieved 2021-09-10.
- ↑ Critcher, Matt S.; Sobczynska-Malefora, Agata (2015-09-15). "Vitamin B6: low and very high concentrations in hospital patients" (PDF). The Biomedical Scientist. Archived from the original (PDF) on 2022-04-08. Retrieved 2019-11-16.
- ↑ "Scientific Opinion on the safety and efficacy of vitamin B6(pyridoxine hydrochloride) as a feed additive for all animal species". EFSA Journal. 9 (5): 2171. 2011. doi: 10.2903/j.efsa.2011.2171 . ISSN 1831-4732.
- ↑ Echaniz-Laguna, Andoni; Mourot-Cottet, Rachel; Noel, Esther; Chanson, Jean-Baptiste (2018). "Regressive pyridoxine-induced sensory neuronopathy in a patient with homocystinuria". BMJ Case Reports. 2018: bcr–2018–225059. doi:10.1136/bcr-2018-225059. ISSN 1757-790X. PMC 6040505 . PMID 29954767.
- 1 2 Gdynia, Hans-Jürgen; Müller, Timo; Sperfeld, Anne-Dorte; Kühnlein, Peter; Otto, Markus; Kassubek, Jan; Ludolph, Albert C. (2008). "Severe sensorimotor neuropathy after intake of highest dosages of vitamin B6". Neuromuscular Disorders. 18 (2): 156–158. doi:10.1016/j.nmd.2007.09.009. ISSN 0960-8966. PMID 18060778. S2CID 7370460.
- ↑ Whyte, M P; Mahuren, J D; Vrabel, L A; Coburn, S P (1985). "Markedly increased circulating pyridoxal-5'-phosphate levels in hypophosphatasia. Alkaline phosphatase acts in vitamin B6 metabolism". Journal of Clinical Investigation. 76 (2): 752–756. doi:10.1172/JCI112031. ISSN 0021-9738. PMC 423894 . PMID 4031070.
- 1 2 Bacharach, Rae; Lowden, Max; Ahmed, Aiesha (2017). "Pyridoxine Toxicity Small Fiber Neuropathy With Dysautonomia". Journal of Clinical Neuromuscular Disease. 19 (1): 43–46. doi:10.1097/CND.0000000000000172. ISSN 1522-0443. PMID 28827489. S2CID 13734173.
- ↑ Bashar Katirji; Henry J. Kaminski; Robert L. Ruff (11 October 2013). Neuromuscular Disorders in Clinical Practice. Springer Science & Business Media. pp. 468–. ISBN 978-1-4614-6567-6. Archived from the original on 19 March 2024. Retrieved 7 December 2019.
- 1 2 Sheikh, S. I.; Amato, A. A. (2010). "The dorsal root ganglion under attack: the acquired sensory ganglionopathies". Practical Neurology. 10 (6): 326–334. doi:10.1136/jnnp.2010.230532. ISSN 1474-7758. PMID 21097829. S2CID 38755244.
- ↑ Perry, Tracy Ann; Weerasuriya, Ananda; Mouton, Peter R.; Holloway, Harold W.; Greig, Nigel H. (2004). "Pyridoxine-induced toxicity in rats: A stereological quantification of the sensory neuropathy". Experimental Neurology. 190 (1): 133–. doi:10.1016/j.expneurol.2004.07.013. PMID 15473987. S2CID 25543353. Archived from the original on 2021-05-12. Retrieved 2020-06-06.
- ↑ Misra, UshaKant; Kalita, Jayantee; Nair, PradeepP (2008). "Diagnostic approach to peripheral neuropathy". Annals of Indian Academy of Neurology. 11 (2): 89–97. doi: 10.4103/0972-2327.41875 . ISSN 0972-2327. PMC 2771953 . PMID 19893645.
- ↑ Bakkers, Mayienne (2015). Small fibers, big troubles: diagnosis and implications of small fiber neuropathy (PDF). Datawyse / Universitaire Pers Maastricht. Archived (PDF) from the original on 2019-10-24. Retrieved 2019-12-01.
- ↑ Hasannejad, Farkhonde; Ansar, Malek Moein; Rostampour, Mohammad; Mahdavi Fikijivar, Edris; Khakpour Taleghani, Behrooz (2019). "Improvement of pyridoxine-induced peripheral neuropathy by Cichorium intybus hydroalcoholic extract through GABAergic system". The Journal of Physiological Sciences. 69 (3): 465–476. doi: 10.1007/s12576-019-00659-8 . ISSN 1880-6546. PMC 10718042 . PMID 30712095. S2CID 59541162.
- ↑ Callizot, Noelle; Warter, Jean-Marie; Poindron, Philippe (2001). "Pyridoxine-Induced Neuropathy in Rats: A Sensory Neuropathy That Responds to 4-Methylcatechol". Neurobiology of Disease. 8 (4): 626–635. doi:10.1006/nbdi.2001.0408. ISSN 0969-9961. PMID 11493027. S2CID 30526195.
- ↑ Hong, Bin Na; Yi, Tae Hoo; Kim, Sun Yeou; Kang, Tong Ho (2009). "High-Dosage Pyridoxine-Induced Auditory Neuropathy and Protection with Coffee in Mice". Biological & Pharmaceutical Bulletin. 32 (4): 597–603. doi: 10.1248/bpb.32.597 . ISSN 0918-6158. PMID 19336890.