Charcot–Marie–Tooth disease (CMT) is a hereditary motor and sensory neuropathy of the peripheral nervous system characterized by progressive loss of muscle tissue and touch sensation across various parts of the body. This disease is the most commonly inherited neurological disorder, affecting about one in 2,500 people. It is named after those who classically described it: the Frenchman Jean-Martin Charcot (1825–1893), his pupil Pierre Marie (1853–1940), and the Briton Howard Henry Tooth (1856–1925).

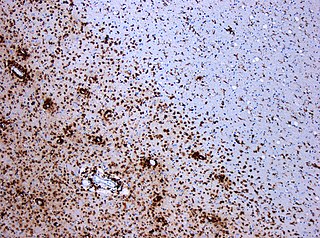
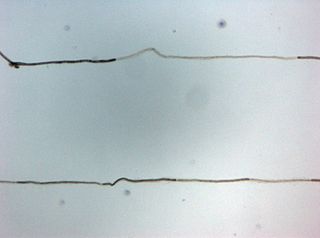
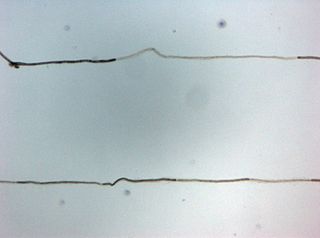
Myelin is a lipid-rich extramembranous structure found on the axons and dendrites of neuron in many bilaterian animals, mainly vertebrates, as well as some arthropods and annelids. A circumferential wrapping of myelin, known as a myelin sheath, increases the conduction speed of electrical impulses passing along the axon by generating saltatory conductions, which are much faster than conduction along an unmyelinated axon, and also reduce signal loss due to extrinsic disturbances.
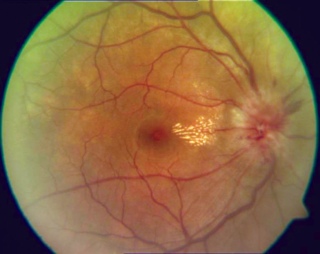
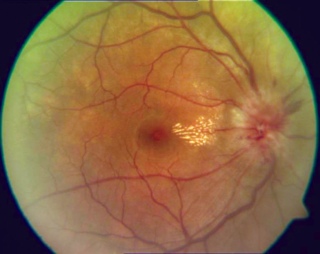
Optic neuritis describes any condition that causes inflammation of the optic nerve; it may be associated with demyelinating diseases, or infectious or inflammatory processes.
Diabetic neuropathy is various types of nerve damage associated with diabetes mellitus. Symptoms depend on the site of nerve damage and can include motor changes such as weakness; sensory symptoms such as numbness, tingling, or pain; or autonomic changes such as urinary symptoms. These changes are thought to result from a microvascular injury involving small blood vessels that supply nerves. Relatively common conditions which may be associated with diabetic neuropathy include distal symmetric polyneuropathy; third, fourth, or sixth cranial nerve palsy; mononeuropathy; mononeuropathy multiplex; diabetic amyotrophy; and autonomic neuropathy.

Peripheral neuropathy, often shortened to neuropathy, is a general term describing damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerves are affected. Neuropathy affecting motor, sensory, or autonomic nerves result in different symptoms. More than one type of nerve may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.
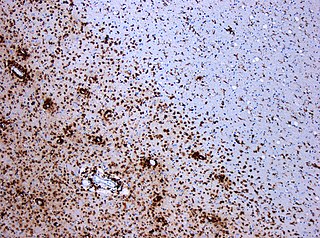
A demyelinating disease refers to any disease affecting the nervous system where the myelin sheath surrounding neurons is damaged. This damage disrupts the transmission of signals through the affected nerves, resulting in a decrease in their conduction ability. Consequently, this reduction in conduction can lead to deficiencies in sensation, movement, cognition, or other functions depending on the nerves affected.

Alcoholic polyneuropathy is a neurological disorder in which peripheral nerves throughout the body malfunction simultaneously. It is defined by axonal degeneration in neurons of both the sensory and motor systems and initially occurs at the distal ends of the longest axons in the body. This nerve damage causes an individual to experience pain and motor weakness, first in the feet and hands and then progressing centrally. Alcoholic polyneuropathy is caused primarily by chronic alcoholism; however, vitamin deficiencies are also known to contribute to its development. This disease typically occurs in chronic alcoholics who have some sort of nutritional deficiency. Treatment may involve nutritional supplementation, pain management, and abstaining from alcohol.

Neuritis is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.
Polyneuropathy in dogs and cats is a collection of peripheral nerve disorders that often are breed-related in these animals. Polyneuropathy indicates that multiple nerves are involved, unlike mononeuropathy. Polyneuropathy usually involves motor nerve dysfunction, also known as lower motor neuron disease. Symptoms include decreased or absent reflexes and muscle tone, weakness, or paralysis. It often occurs in the rear legs and is bilateral. Most are chronic problems with a slow onset of symptoms, but some occur suddenly.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired autoimmune disease of the peripheral nervous system characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder is sometimes called chronic relapsing polyneuropathy (CRP) or chronic inflammatory demyelinating polyradiculoneuropathy. CIDP is closely related to Guillain–Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. It is one of several types of neuropathy.
Small fiber peripheral neuropathy is a type of peripheral neuropathy that occurs from damage to the small unmyelinated and myelinated peripheral nerve fibers. These fibers, categorized as C fibers and small Aδ fibers, are present in skin, peripheral nerves, and organs. The role of these nerves is to innervate some skin sensations and help control autonomic function. It is estimated that 15–20 million people in the United States have some form of peripheral neuropathy.
Guillain–Barré syndrome (GBS) is a rapid-onset muscle weakness caused by the immune system damaging the peripheral nervous system. Typically, both sides of the body are involved, and the initial symptoms are changes in sensation or pain often in the back along with muscle weakness, beginning in the feet and hands, often spreading to the arms and upper body. The symptoms may develop over hours to a few weeks. During the acute phase, the disorder can be life-threatening, with about 15% of people developing weakness of the breathing muscles and, therefore, requiring mechanical ventilation. Some are affected by changes in the function of the autonomic nervous system, which can lead to dangerous abnormalities in heart rate and blood pressure.
Antiganglioside antibodies that react to self-gangliosides are found in autoimmune neuropathies. These antibodies were first found to react with cerebellar cells. These antibodies show highest association with certain forms of Guillain–Barré syndrome.
Critical illness polyneuropathy (CIP) and critical illness myopathy (CIM) are overlapping syndromes of diffuse, symmetric, flaccid muscle weakness occurring in critically ill patients and involving all extremities and the diaphragm with relative sparing of the cranial nerves. CIP and CIM have similar symptoms and presentations and are often distinguished largely on the basis of specialized electrophysiologic testing or muscle and nerve biopsy. The causes of CIP and CIM are unknown, though they are thought to be a possible neurological manifestation of systemic inflammatory response syndrome. Corticosteroids and neuromuscular blocking agents, which are widely used in intensive care, may contribute to the development of CIP and CIM, as may elevations in blood sugar, which frequently occur in critically ill patients.
Progressive inflammatory neuropathy is a disease that was identified in a report, released on January 31, 2008, by the Centers for Disease Control and Prevention. The first known outbreak of this neuropathy occurred in southeastern Minnesota in the United States. The disease was reported among pig slaughterhouse workers who appeared at various care facilities in the area reporting similar neurological symptoms. The disease was later identified at pork processing plants in Indiana and Nebraska as well. The condition is characterized by acute paralysis, pain, fatigue, numbness, and weakness, especially in extremities. It was initially believed that workers might have contracted the disease through inhaling aerosols from pig brains blown through a compressed-air hose and that this exposure to pig neural tissue induced an autoimmune response that might have produced their mysterious peripheral neuropathy. These suspicions were confirmed in reports and investigations conducted at the Mayo Clinic in Rochester, Minnesota.

Hereditary motor and sensory neuropathies (HMSN) is a name sometimes given to a group of different neuropathies which are all characterized by their impact upon both afferent and efferent neural communication. HMSN are characterised by atypical neural development and degradation of neural tissue. The two common forms of HMSN are either hypertrophic demyelinated nerves or complete atrophy of neural tissue. Hypertrophic condition causes neural stiffness and a demyelination of nerves in the peripheral nervous system, and atrophy causes the breakdown of axons and neural cell bodies. In these disorders, a patient experiences progressive muscle atrophy and sensory neuropathy of the extremities.
Anti-MAG peripheral neuropathy is a specific type of peripheral neuropathy in which the person's own immune system attacks cells that are specific in maintaining a healthy nervous system. As these cells are destroyed by antibodies, the nerve cells in the surrounding region begin to lose function and create many problems in both sensory and motor function. Specifically, antibodies against myelin-associated glycoprotein (MAG) damage Schwann cells. While the disorder occurs in only 10% of those afflicted with peripheral neuropathy, people afflicted have symptoms such as muscle weakness, sensory problems, and other motor deficits usually starting in the form of a tremor of the hands or trouble walking. There are, however, multiple treatments that range from simple exercises in order to build strength to targeted drug treatments that have been shown to improve function in people with this type of peripheral neuropathy.
Multifocal motor neuropathy (MMN) is a progressively worsening condition where muscles in the extremities gradually weaken. The disorder, a pure motor neuropathy syndrome, is sometimes mistaken for amyotrophic lateral sclerosis (ALS) because of the similarity in the clinical picture, especially if muscle fasciculations are present. MMN is thought to be autoimmune. It was first described in the mid-1980s.
Peripheral mononeuropathy is a nerve related disease where a single nerve, that is used to transport messages from the brain to the peripheral body, is diseased or damaged. Peripheral neuropathy is a general term that indicates any disorder of the peripheral nervous system. The name of the disorder itself can be broken down in order to understand this better; peripheral: in regard to peripheral neuropathy, refers to outside of the brain and spinal cord; neuro: means nerve related; -pathy; means disease. Peripheral mononeuropathy is a disorder that links to Peripheral Neuropathy, as it only effects a single peripheral nerve rather than several damaged or diseased nerves throughout the body. Healthy peripheral nerves are able to “carry messages from the brain and spinal cord to muscles, organs, and other body tissues”.