Related Research Articles

A nerve is an enclosed, cable-like bundle of nerve fibers in the peripheral nervous system.

Cranial nerves are the nerves that emerge directly from the brain, of which there are conventionally considered twelve pairs. Cranial nerves relay information between the brain and parts of the body, primarily to and from regions of the head and neck, including the special senses of vision, taste, smell, and hearing.

The parasympathetic nervous system (PSNS) is one of the three divisions of the autonomic nervous system, the others being the sympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.

The brainstem is the stalk-like part of the brain that interconnects the cerebrum and diencephalon with the spinal cord. In the human brain, the brainstem is composed of the midbrain, the pons, and the medulla oblongata. The midbrain is continuous with the thalamus of the diencephalon through the tentorial notch.

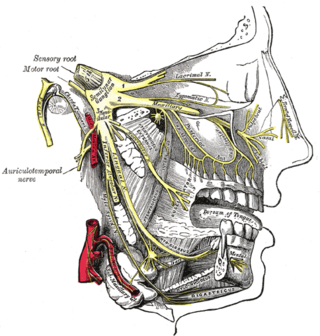
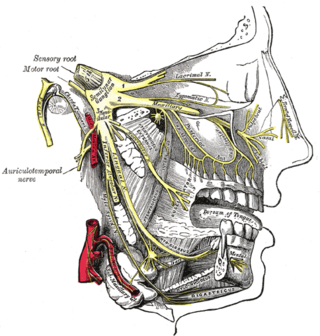
In neuroanatomy, the trigeminal nerve (lit. triplet nerve), also known as the fifth cranial nerve, cranial nerve V, or simply CN V, is a cranial nerve responsible for sensation in the face and motor functions such as biting and chewing; it is the most complex of the cranial nerves. Its name (trigeminal, from Latin tri- 'three', and -geminus 'twin') derives from each of the two nerves (one on each side of the pons) having three major branches: the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3). The ophthalmic and maxillary nerves are purely sensory, whereas the mandibular nerve supplies motor as well as sensory (or "cutaneous") functions. Adding to the complexity of this nerve is that autonomic nerve fibers as well as special sensory fibers (taste) are contained within it.
Trigeminal neuralgia, also called Fothergill disease, tic douloureux, trifacial neuralgia, or suicide disease is a long-term pain disorder that affects the trigeminal nerve, the nerve responsible for sensation in the face and motor functions such as biting and chewing. It is a form of neuropathic pain. There are two main types: typical and atypical trigeminal neuralgia. The typical form results in episodes of severe, sudden, shock-like pain in one side of the face that lasts for seconds to a few minutes. Groups of these episodes can occur over a few hours. The atypical form results in a constant burning pain that is less severe. Episodes may be triggered by any touch to the face. Both forms may occur in the same person. It is regarded as one of the most painful disorders known to medicine, and often results in depression and suicide.

A nociceptor is a sensory neuron that responds to damaging or potentially damaging stimuli by sending "possible threat" signals to the spinal cord and the brain. The brain creates the sensation of pain to direct attention to the body part, so the threat can be mitigated; this process is called nociception.

The solitary nucleus is a series of sensory nuclei forming a vertical column of grey matter in the medulla oblongata of the brainstem. It receives general visceral and/or special visceral inputs from the facial nerve, glossopharyngeal nerve and vagus nerve ; it receives and relays stimuli related to taste and visceral sensation. It sends outputs to various parts of the brain, such as the hypothalamus, thalamus, and reticular formation. Neuron cell bodies of the SN are roughly somatotopically arranged along its length according to function.
Postherpetic neuralgia (PHN) is neuropathic pain that occurs due to damage to a peripheral nerve caused by the reactivation of the varicella zoster virus. PHN is defined as pain in a dermatomal distribution that lasts for at least 90 days after an outbreak of herpes zoster. Several types of pain may occur with PHN including continuous burning pain, episodes of severe shooting or electric-like pain, and a heightened sensitivity to gentle touch which would not otherwise cause pain or to painful stimuli. Abnormal sensations and itching may also occur.
Neuropathic pain is pain caused by a lesion or disease of the somatosensory nervous system. Neuropathic pain may be associated with abnormal sensations called dysesthesia or pain from normally non-painful stimuli (allodynia). It may have continuous and/or episodic (paroxysmal) components. The latter resemble stabbings or electric shocks. Common qualities include burning or coldness, "pins and needles" sensations, numbness and itching.

Headshaking is a behaviour displayed by horses, where the horse continuously shakes its head vertically and/or horizontally. In the 1980s it was considered a bad behaviour, but instead it turned out to be a painful medical condition.

Nerve injury is an injury to a nerve. There is no single classification system that can describe all the many variations of nerve injuries. In 1941, Seddon introduced a classification of nerve injuries based on three main types of nerve fiber injury and whether there is continuity of the nerve. Usually, however, nerve injuries are classified in five stages, based on the extent of damage to both the nerve and the surrounding connective tissue, since supporting glial cells may be involved.

The cranial nerve exam is a type of neurological examination. It is used to identify problems with the cranial nerves by physical examination. It has nine components. Each test is designed to assess the status of one or more of the twelve cranial nerves (I-XII). These components correspond to testing the sense of smell (I), visual fields and acuity (II), eye movements and pupils, sensory function of face (V), strength of facial (VII) and shoulder girdle muscles (XI), hearing and balance, taste, pharyngeal movement and reflex, tongue movements (XII).
Geniculate ganglionitis or geniculate neuralgia (GN), also called nervus intermedius neuralgia, Ramsay Hunt syndrome, or Hunt's neuralgia, is a rare disorder characterized by severe paroxysmal neuralgic pain deep in the ear, that may spread to the ear canal, outer ear, mastoid or eye regions. GN may also occur in combination with trigeminal or glossopharyngeal neuralgia.

Group C nerve fibers are one of three classes of nerve fiber in the central nervous system (CNS) and peripheral nervous system (PNS). The C group fibers are unmyelinated and have a small diameter and low conduction velocity, whereas Groups A and B are myelinated. Group C fibers include postganglionic fibers in the autonomic nervous system (ANS), and nerve fibers at the dorsal roots. These fibers carry sensory information.

The gustatory nucleus is the rostral part of the solitary nucleus located in the medulla. The gustatory nucleus is associated with the sense of taste and has two sections, the rostral and lateral regions. A close association between the gustatory nucleus and visceral information exists for this function in the gustatory system, assisting in homeostasis - via the identification of food that might be possibly poisonous or harmful for the body. There are many gustatory nuclei in the brain stem. Each of these nuclei corresponds to three cranial nerves, the facial nerve (VII), the glossopharyngeal nerve (IX), and the vagus nerve (X) and GABA is the primary inhibitory neurotransmitter involved in its functionality. All visceral afferents in the vagus and glossopharyngeal nerves first arrive in the nucleus of the solitary tract and information from the gustatory system can then be relayed to the thalamus and cortex.
Atypical trigeminal neuralgia (ATN), or type 2 trigeminal neuralgia, is a form of trigeminal neuralgia, a disorder of the fifth cranial nerve. This form of nerve pain is difficult to diagnose, as it is rare and the symptoms overlap with several other disorders. The symptoms can occur in addition to having migraine headache, or can be mistaken for migraine alone, or dental problems such as temporomandibular joint disorder or musculoskeletal issues. ATN can have a wide range of symptoms and the pain can fluctuate in intensity from mild aching to a crushing or burning sensation, and also to the extreme pain experienced with the more common trigeminal neuralgia.

The wide dynamic range (WDR) neuron was first discovered by Mendell in 1966. Early studies of this neuron established what is known as the gate control theory of pain. The basic concept is that non-painful stimuli block the pathways for painful stimuli, inhibiting possible painful responses. This theory was supported by the fact that WDR neurons are responsible for responses to both painful and non-painful stimuli, and the idea that these neurons could not produce more than one of these responses simultaneously. WDR neurons respond to all types of somatosensory stimuli, make up the majority of the neurons found in the posterior grey column, and have the ability to produce long range responses including those responsible for pain and itch.
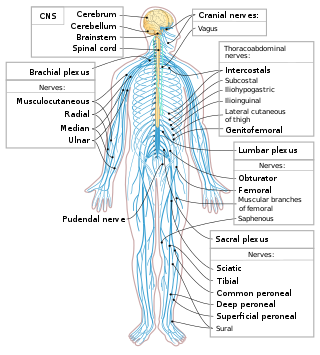
The following diagram is provided as an overview of and topical guide to the human nervous system:
Ocular neuropathic pain is a spectrum of disorders of ocular pain which are caused by damage or disease affecting the nerves. Ocular neuropathic pain is frequently associated with damaged or dysfunctional corneal nerves, but the condition can also be caused by peripheral or centralized sensitization. The condition shares some characteristics with somatic neuropathic pain in that it is similarly associated with abnormal sensations (dysesthesia) or pain from normally non-painful stimuli (allodynia), but until recent years has been poorly understood by the medical community, and frequently dismissed by ophthalmologists who were not trained to identify neuropathic pain as a source of unexplained eye pain beyond objective findings noted on slit-lamp examination.
References
- ↑ "IASP Terminology: neuralgia". International Association for the Study of Pain . Retrieved 15 Nov 2023.
- 1 2 3 4 Gilron, I.; Watson, C. P. N.; Cahill, C. M.; Moulin, D. E. (2006). "Neuropathic pain: a practical guide for the clinician". Canadian Medical Association Journal. 175 (3): 265–275. doi:10.1503/cmaj.060146. PMC 1513412 . PMID 16880448.
- 1 2 Jensen, T. S. (2002). "An improved understanding of neuropathic pain". European Journal of Pain. London. 6 (Supplement): 3–11. doi:10.1016/S1090-3801(02)90002-9. PMID 23570142. S2CID 12760893.
- 1 2 3 P. Prithvi Raj (14 June 2000). Practical Management of Pain . Mosby. ISBN 978-0-8151-2569-3.
- ↑ Melzack, R. (1975). "The McGill Questionnaire: Major Properties and Scoring Methods". Pain. 1 (3): 277–299. doi:10.1016/0304-3959(75)90044-5. PMID 1235985. S2CID 20562841.
- ↑ Garcia-Larrea, L. (2008). "Laser-evoked potentials in the diagnosis of central neuropathic pain". Douleur et Analgésie. 21 (2): 93–98. doi:10.1007/s11724-008-0092-5. S2CID 70895743.
- ↑ Daniel, H. C.; Narewska, J.; Serpell, M.; Hoggart, B.; Johnson, R.; Rice, A. S. C. (2008). "Comparison of psychological and physical function in neuropathic pain and nociceptive pain: Implications for cognitive behavioral pain management programs". European Journal of Pain. 12 (6): 731–741. doi:10.1016/j.ejpain.2007.11.006. PMID 18164225. S2CID 28750350.
- 1 2 Stechison, Michael. Personal INTERVIEW. 18 November 2008.
- ↑ Galer, B. S. (1995). "Neuropathic pain of peripheral origin: Advances in pharmacologic treatment". Neurology. 45 (129): S17–S25. doi:10.1212/WNL.45.12_Suppl_9.S17. PMID 8538882. S2CID 38518116.
- ↑ Dworkin, R. H.; Backonja, M.; Rowbotham, M. C.; Allen, R. R.; Argoff, C. R.; Bennett, GJ; Bushnell, MC; Farrar, JT; et al. (2003). "Advances in neuropathic pain - Diagnosis, mechanisms, and treatment recommendations". Archives of Neurology. 60 (11): 1524–1534. doi: 10.1001/archneur.60.11.1524 . PMID 14623723.
- ↑ Murray JAH. Bradley H; Craigie WA; Onions CT (1933). Oxford English Dictionary. Clarendon Press.
- ↑ Richard Rowland (1838). A treatise on neuralgia. p. 3 . Retrieved 5 August 2012.
- 1 2 3 Alam C & Merskey H (1994). "What's in a name? The cycle of change in the meaning of neuralgia". History of Psychiatry. 5 (20): 429–474. doi:10.1177/0957154x9400502001. PMID 11639457. S2CID 11856642.
- ↑ Warren JC (19 February 1928). "Cases of neuralgia or painful afflictions of the nerves". Boston Med. Surg. J. (i): 1–6.
- ↑ Graham TJ (1928). Treatise on indigestion. London: W. Joy. pp. 256–7.
- ↑ Teale TP (1830). A treatise on neuralgic diseases. Philadelphia: E. L. Carey & A. Hart.
- ↑ Sherriff, Robert Cedric (1983). Journey's end. Harmondsworth: Penguin. pp. 53–58. ISBN 0-14-118326-8.
- ↑ Aces High. 1976. Event occurs at 12:39.