Related Research Articles

Spinal muscular atrophies (SMAs) are a genetically and clinically heterogeneous group of rare debilitating disorders characterised by the degeneration of lower motor neurons and subsequent atrophy (wasting) of various muscle groups in the body. While some SMAs lead to early infant death, other diseases of this group permit normal adult life with only mild weakness.
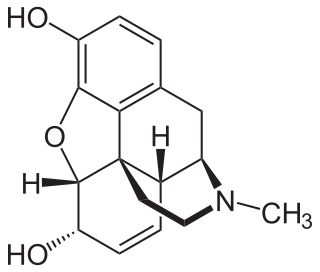
Opioid use disorder (OUD) is a substance use disorder characterized by cravings for opioids, continued use despite physical and/or psychological deterioration, increased tolerance with use, and withdrawal symptoms after discontinuing opioids. Opioid withdrawal symptoms include nausea, muscle aches, diarrhea, trouble sleeping, agitation, and a low mood. Addiction and dependence are important components of opioid use disorder.

Buprenorphine, sold under the brand name Subutex among others, is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, the patient must have moderate opioid withdrawal symptoms before buprenorphine can be administered under direct observation of a health-care provider.

Erythromelalgia or Mitchell's disease is a rare vascular peripheral pain disorder in which blood vessels, usually in the lower extremities or hands, are episodically blocked, then become hyperemic and inflamed. There is severe burning pain and skin redness. The attacks are periodic and are commonly triggered by heat, pressure, mild activity, exertion, insomnia or stress. Erythromelalgia may occur either as a primary or secondary disorder. Secondary erythromelalgia can result from small fiber peripheral neuropathy of any cause, polycythemia vera, essential thrombocythemia, hypercholesterolemia, mushroom or mercury poisoning, and some autoimmune disorders. Primary erythromelalgia is caused by mutation of the voltage-gated sodium channel α-subunit gene SCN9A.

Congenital insensitivity to pain with anhidrosis (CIPA) is a rare autosomal recessive disorder of the nervous system which prevents the feeling of pain or temperature, and prevents a person from sweating. Cognitive disorders are commonly coincident. CIPA is the fourth type of hereditary sensory and autonomic neuropathy (HSAN), and is also known as HSAN IV.

The periaqueductal gray is a brain region that plays a critical role in autonomic function, motivated behavior and behavioural responses to threatening stimuli. PAG is also the primary control center for descending pain modulation. It has enkephalin-producing cells that suppress pain.

Fatty-acid amide hydrolase 1 (FAAH) is a member of the serine hydrolase family of enzymes. It was first shown to break down anandamide (AEA), an N-acylethanolamine (NAE) in 1993. In humans, it is encoded by the gene FAAH.
Small fiber peripheral neuropathy is a type of peripheral neuropathy that occurs from damage to the small unmyelinated and myelinated peripheral nerve fibers. These fibers, categorized as C fibers and small Aδ fibers, are present in skin, peripheral nerves, and organs. The role of these nerves is to innervate some skin sensations and help control autonomic function. It is estimated that 15–20 million people in the United States have some form of peripheral neuropathy.

Nav1.7 is a sodium ion channel that in humans is encoded by the SCN9A gene. It is usually expressed at high levels in two types of neurons: the nociceptive (pain) neurons at the dorsal root ganglion (DRG) and trigeminal ganglion; and sympathetic ganglion neurons, which are part of the autonomic (involuntary) nervous system.

Sodium channel, voltage-gated, type XI, alpha subunit also known as SCN11A or Nav1.9 is a voltage-gated sodium ion channel protein which is encoded by the SCN11A gene on chromosome 3 in humans. Like Nav1.7 and Nav1.8, Nav1.9 plays a role in pain perception. This channel is largely expressed in small-diameter nociceptors of the dorsal root ganglion and trigeminal ganglion neurons, but is also found in intrinsic myenteric neurons.
Paroxysmal extreme pain disorder originally named familial rectal pain syndrome, is a rare disorder whose most notable features are pain in the mandibular, ocular and rectal areas as well as flushing. PEPD often first manifests at the beginning of life, perhaps even in utero, with symptoms persisting throughout life. PEPD symptoms are reminiscent of primary erythromelalgia, as both result in flushing and episodic pain, though pain is typically present in the extremities for primary erythromelalgia. Both of these disorders have recently been shown to be allelic, both caused by mutations in the voltage-gated sodium channel NaV1.7 encoded by the gene SCN9A. A different mutation in the SCN9A ion channel causes congenital insensitivity to pain.
Hereditary sensory and autonomic neuropathy (HSAN) or hereditary sensory neuropathy (HSN) is a condition used to describe any of the types of this disease which inhibit sensation.
Hereditary sensory neuropathy, type II also known as HSN2 is a region of a parent protein which in humans is encoded by the WNK1 gene. It is a transcript variant of the WNK1 gene that is selectively expressed in nervous system tissues, and during development. Mutations in this exon of the WNK1 gene have been identified as causative in genetic neuropathy syndromes, and in inherited pain insensitivity.

Nav1.8 is a sodium ion channel subtype that in humans is encoded by the SCN10A gene.
Hereditary sensory and autonomic neuropathy type I or hereditary sensory neuropathy type I is a group of autosomal dominant inherited neurological diseases that affect the peripheral nervous system particularly on the sensory and autonomic functions. The hallmark of the disease is the marked loss of pain and temperature sensation in the distal parts of the lower limbs. The autonomic disturbances, if present, manifest as sweating abnormalities.

PR domain zinc finger protein 12 is a protein that in humans is encoded by the PRDM12 gene. This gene is normally switched on during the development of pain-sensing nerve cells. People with homozygous mutations of the PRDM12 gene experience congenital insensitivity to pain (CIP). PRMD12 is a part of a larger domain that mediate histone methyltransferases. Enzymes target gene promoters in order to control gene expression.

Zinc finger homeobox 2 is a protein that in humans is encoded by the ZFHX2 gene. It has been implicated in pain insensitivity.
The eradication or abolition of suffering is the concept of using biotechnology to create a permanent absence of involuntary pain and suffering in all sentient beings.

17q12 microdeletion syndrome, also known as 17q12 deletion syndrome, is a rare chromosomal anomaly caused by the deletion of a small amount of material from a region in the long arm of chromosome 17. It is typified by deletion of the HNF1B gene, resulting in kidney abnormalities and renal cysts and diabetes syndrome. It also has neurocognitive effects, and has been implicated as a genetic factor for autism and schizophrenia.

Marsili syndrome is an extremely rare genetic disorder which is characterized by symptoms similar to those reported on individuals with congenital insensitivity to pain with anhidrosis. It can be fatal if it goes unnoticed/undiagnosed.
References
- 1 2 3 4 Linton S (2005). Understanding Pain for Better Clinical Practice: A Psychological Perspective. Elsevier Health Sciences. p. 14. ISBN 978-0444515919 . Retrieved April 13, 2017.
- 1 2 3 4 Hellier JL (2016). The Five Senses and Beyond: The Encyclopedia of Perception. ABC-CLIO. pp. 118–119. ISBN 978-1440834172 . Retrieved April 13, 2017.
- ↑ Online Mendelian Inheritance in Man (OMIM): Insensitivity to Pain, Congenital, with Anhidrosis; CIPA - 256800
- 1 2 Brodsky MC (2016). Pediatric Neuro-Ophthalmology. Springer. p. 741. ISBN 978-1493933846 . Retrieved April 13, 2017.
- ↑ Manfredi M, Bini G, Cruccu G, Accornero N, Berardelli A, Medolago L (August 1981). "Congenital absence of pain". Archives of Neurology. 38 (8): 507–11. doi:10.1001/archneur.1981.00510080069010. PMID 6166287.
- ↑ Bennett DL, Clark AJ, Huang J, Waxman SG, Dib-Hajj SD (April 2019). "The Role of Voltage-Gated Sodium Channels in Pain Signaling". Physiological Reviews. 99 (2): 1079–1151. doi: 10.1152/physrev.00052.2017 . PMID 30672368.
- ↑ Cox JJ, Reimann F, Nicholas AK, Thornton G, Roberts E, Springell K, et al. (December 2006). "An SCN9A channelopathy causes congenital inability to experience pain". Nature. 444 (7121): 894–8. Bibcode:2006Natur.444..894C. doi:10.1038/nature05413. PMC 7212082 . PMID 17167479.
- ↑ McDermott LA, Weir GA, Themistocleous AC, Segerdahl AR, Blesneac I, Baskozos G, Clark AJ, Millar V, Peck LJ, Ebner D, Tracey I, Serra J, Bennett DL (March 2019). "V1.7 in Human Nociception". Neuron. 101 (5): 905–919.e8. doi:10.1016/j.neuron.2019.01.047. PMC 6424805 . PMID 30795902.
- ↑ Chen YC, Auer-Grumbach M, Matsukawa S, Zitzelsberger M, Themistocleous AC, Strom TM, et al. (July 2015). "Transcriptional regulator PRDM12 is essential for human pain perception". Nature Genetics. 47 (7): 803–8. doi:10.1038/ng.3308. hdl: 2262/75983 . PMC 7212047 . PMID 26005867.
- ↑ Costandi M (2015-05-25). "Uncomfortably numb: The people who feel no pain". the guardian. Retrieved 31 July 2015.
- ↑ Murphy H (2019-03-28). "At 71, She's Never Felt Pain or Anxiety. Now Scientists Know Why". The New York Times. ISSN 0362-4331 . Retrieved 2019-03-30.
- ↑ Habib AM, Okorokov AL, Hill MN, Bras JT, Lee MC, Li S, Gossage SJ, van Drimmelen M, Morena M, Houlden H, Ramirez JD, Bennett DL, Srivastava D, Cox JJ (22 February 2019). "Microdeletion in a FAAH pseudogene identified in a patient with high anandamide concentrations and pain insensitivity". British Journal of Anaesthesia. 123 (2): e249–e253. doi:10.1016/j.bja.2019.02.019. PMC 6676009 . PMID 30929760.
- ↑ Habib, Abdella M.; Matsuyama, Ayako; Okorokov, Andrei L.; Santana-Varela, Sonia; Bras, Jose T.; Aloisi, Anna Maria; Emery, Edward C.; Bogdanov, Yury D.; Follenfant, Maryne; Gossage, Sam J.; Gras, Mathilde (2018-02-01). "A novel human pain insensitivity disorder caused by a point mutation in ZFHX2". Brain: A Journal of Neurology. 141 (2): 365–376. doi:10.1093/brain/awx326. ISSN 1460-2156. PMC 5837393 . PMID 29253101.
- ↑ Wolraich M (2008). Developmental-behavioral Pediatrics: Evidence and Practice. Elsevier Health Sciences. p. 399. ISBN 9780323040259.
- 1 2 3 Minett MS, Pereira V, Sikandar S, Matsuyama A, Lolignier S, Kanellopoulos AH, Mancini F, Iannetti GD, Bogdanov YD, Santana-Varela S, Millet Q, Baskozos G, MacAllister R, Cox JJ, Zhao J, Wood JN (December 2015). "Endogenous opioids contribute to insensitivity to pain in humans and mice lacking sodium channel Nav1.7". Nature Communications. 6 (1): 8967. Bibcode:2015NatCo...6.8967M. doi:10.1038/ncomms9967. PMC 4686868 . PMID 26634308.
- ↑ KARIMI, Mehran; LLAH, Razieh FA (Summer 2012). "A Case Report of Congenital Insensitivity to Pain and Anhidrosis (CIPA)". Iranian Journal of Child Neurology. 6 (3): 45–48. PMC 3943025 . PMID 24665272.
- ↑ Minde JK (April 2006). "Norrbottnian congenital insensitivity to pain". Acta Orthopaedica. Supplementum. 77 (321): 2–32. PMID 16768023.