Split-brain or callosal syndrome is a type of disconnection syndrome when the corpus callosum connecting the two hemispheres of the brain is severed to some degree. It is an association of symptoms produced by disruption of, or interference with, the connection between the hemispheres of the brain. The surgical operation to produce this condition involves transection of the corpus callosum, and is usually a last resort to treat refractory epilepsy. Initially, partial callosotomies are performed; if this operation does not succeed, a complete callosotomy is performed to mitigate the risk of accidental physical injury by reducing the severity and violence of epileptic seizures. Before using callosotomies, epilepsy is instead treated through pharmaceutical means. After surgery, neuropsychological assessments are often performed.

Myoclonus is a brief, involuntary, irregular twitching of a muscle or a group of muscles. It describes a medical sign and, generally, is not a diagnosis of a disease. These myoclonic twitches, jerks, or seizures are usually caused by sudden muscle contractions or brief lapses of contraction. The most common circumstance under which they occur is while falling asleep. Myoclonic jerks occur in healthy people and are experienced occasionally by everyone. However, when they appear with more persistence and become more widespread they can be a sign of various neurological disorders. Hiccups are a kind of myoclonic jerk specifically affecting the diaphragm. When a spasm is caused by another person it is known as a provoked spasm. Shuddering attacks in babies fall in this category.

Focal cortical dysplasia (FCD) is a congenital abnormality of brain development where the neurons in an area of the brain failed to migrate in the proper formation in utero. Focal means that it is limited to a focal zone in any lobe. Focal cortical dysplasia is a common cause of intractable epilepsy in children and is a frequent cause of epilepsy in adults. There are three types of FCD with subtypes, including type 1a, 1b, 1c, 2a, 2b, 3a, 3b, 3c, and 3d, each with distinct histopathological features. All forms of focal cortical dysplasia lead to disorganization of the normal structure of the cerebral cortex. Type 1 FCD exhibits subtle alterations in cortical lamination. Type 2a FCD exhibits neurons that are larger than normal that are called dysmorphic neurons (DN). FCD type 2b exhibits complete loss of laminar structure, and the presence of DN and enlarged cells are called balloon cells (BC) for their large elliptical cell body shape, laterally displaced nucleus, and lack of dendrites or axons. The developmental origin of balloon cells is currently believed to be derived from neuronal or glial progenitor cells. Balloon cells are similar in structure to giant cells in the disorder tuberous sclerosis complex. Type 3 FCDs are cortical disorganisation associated with other lesions such as hippocampal sclerosis, long-term epilepsy-associated tumors (3b), vascular malformations (3c) or scar/hypoxic damages (3d).
The Wada test, also known as the intracarotid sodium amobarbital procedure (ISAP) establishes cerebral language and memory representation of each hemisphere.
Hemispherectomy is a very rare neurosurgical procedure in which a cerebral hemisphere is removed, disconnected, or disabled. This procedure is used to treat a variety of seizure disorders where the source of the epilepsy is localized to a broad area of a single hemisphere of the brain, notably Rasmussen's encephalitis. About one in three patients with epilepsy will continue to have persistent seizures despite epileptic drug therapy. Hemispherectomy is reserved for the most extreme cases of this one-third in which the individual’s seizures are irresponsive to medications or other less invasive surgeries and significantly impair functioning or put the patient at risk of further complications. The procedure successfully cures seizures in about 85–90% of patients. Additionally, it is also known to often markedly improve the cognitive functioning and development of the individual. Subtotal hemispherectomy sparing sensorimotor cortex can be performed with successful seizure control expected in 70–80% of patients. Even with the presence of widespread unilateral epileptogenicity or anatomic/functional imaging abnormalities, complete hemispherectomy can often be avoided, particularly when there is little hemiparesis.
Epilepsia partialis continua is a rare type of brain disorder in which a patient experiences recurrent motor epileptic seizures that are focal, and recur every few seconds or minutes for extended periods.
Landau–Kleffner syndrome (LKS)—also called infantile acquired aphasia, acquired epileptic aphasia or aphasia with convulsive disorder—is a rare childhood neurological syndrome.

Temporal lobe epilepsy (TLE) is a chronic disorder of the nervous system characterized by recurrent, unprovoked focal seizures that originate in the temporal lobe of the brain and last about one or two minutes. TLE is the most common form of epilepsy with focal seizures. A focal seizure in the temporal lobe may spread to other areas in the brain when it may become a focal to bilateral seizure.
Frontal lobe epilepsy (FLE) is a neurological disorder that is characterized by brief, recurring seizures that arise in the frontal lobes of the brain, often while the patient is sleeping. It is the second most common type of epilepsy after temporal lobe epilepsy (TLE), and is related to the temporal form by the fact that both forms are characterized by the occurrence of partial (focal) seizures. Partial seizures occurring in the frontal lobes can occur in one of two different forms: either simple partial seizures or complex partial seizures. The symptoms and clinical manifestations of frontal lobe epilepsy can differ depending on which specific area of the frontal lobe is affected.
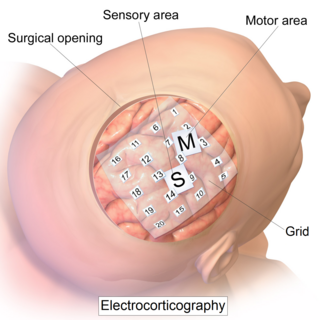
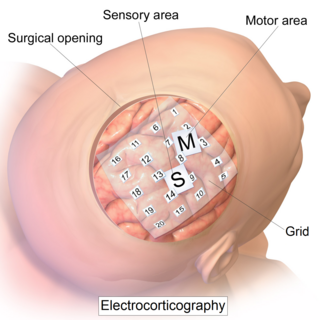
Electrocorticography (ECoG), or intracranial electroencephalography (iEEG), is a type of electrophysiological monitoring that uses electrodes placed directly on the exposed surface of the brain to record electrical activity from the cerebral cortex. In contrast, conventional electroencephalography (EEG) electrodes monitor this activity from outside the skull. ECoG may be performed either in the operating room during surgery or outside of surgery. Because a craniotomy is required to implant the electrode grid, ECoG is an invasive procedure.
Anterior temporal lobectomy is the complete removal of the anterior portion of the temporal lobe of the brain. It is a treatment option in temporal lobe epilepsy for those in whom anticonvulsant medications do not control epileptic seizures.
Epilepsy surgery involves a neurosurgical procedure where an area of the brain involved in seizures is either resected, disconnected or stimulated. The goal is to eliminate seizures or significantly reduce seizure burden. Approximately 60% of all people with epilepsy have focal epilepsy syndromes. In 15% to 20% of these patients, the condition is not adequately controlled with anticonvulsive drugs. Such patients are potential candidates for surgical epilepsy treatment.
A generalized tonic–clonic seizure, commonly known as a grand mal seizure or GTCS, is a type of generalized seizure that produces bilateral, convulsive tonic and clonic muscle contractions. Tonic–clonic seizures are the seizure type most commonly associated with epilepsy and seizures in general and the most common seizure associated with metabolic imbalances. It is a misconception that they are the sole type of seizure, as they are the main seizure type in approximately 10% of those with epilepsy.
Post-traumatic epilepsy (PTE) is a form of acquired epilepsy that results from brain damage caused by physical trauma to the brain. A person with PTE suffers repeated post-traumatic seizures more than a week after the initial injury. PTE is estimated to constitute 5% of all cases of epilepsy and over 20% of cases of acquired epilepsy.
Post-traumatic seizures (PTS) are seizures that result from traumatic brain injury (TBI), brain damage caused by physical trauma. PTS may be a risk factor for post-traumatic epilepsy (PTE), but a person who has a seizure or seizures due to traumatic brain injury does not necessarily have PTE, which is a form of epilepsy, a chronic condition in which seizures occur repeatedly. However, "PTS" and "PTE" may be used interchangeably in medical literature.
Cortical stimulation mapping (CSM) is a type of electrocorticography that involves a physically invasive procedure and aims to localize the function of specific brain regions through direct electrical stimulation of the cerebral cortex. It remains one of the earliest methods of analyzing the brain and has allowed researchers to study the relationship between cortical structure and systemic function. Cortical stimulation mapping is used for a number of clinical and therapeutic applications, and remains the preferred method for the pre-surgical mapping of the motor cortex and language areas to prevent unnecessary functional damage. There are also some clinical applications for cortical stimulation mapping, such as the treatment of epilepsy.

Ulegyria is a diagnosis used to describe a specific type of cortical scarring in the deep regions of the sulcus that leads to distortion of the gyri. Ulegyria is identified by its characteristic "mushroom-shaped" gyri, in which scarring causes shrinkage and atrophy in the deep sulcal regions while the surface gyri are spared. This condition is most often caused by hypoxic-ischemic brain injury in the perinatal period. The effects of ulegyria can range in severity, although it is most commonly associated with cerebral palsy, mental retardation and epilepsy. N.C. Bresler was the first to view ulegyria in 1899 and described this abnormal morphology in the brain as “mushroom-gyri." Although ulegyria was first identified in 1899, there is still limited information known or reported about the condition.
Awake craniotomy is a neurosurgical technique and type of craniotomy that allows a surgeon to remove a brain tumor while the patient is awake to avoid brain damage. During the surgery, the neurosurgeon performs cortical mapping to identify vital areas, called the "eloquent brain", that should not be disturbed while removing the tumor.
Drug-resistant epilepsy (DRE), also known as refractory epilepsy or pharmacoresistant epilepsy, is defined as failure of adequate trials of two tolerated and appropriately chosen and used antiepileptic drugs to achieve sustained seizure freedom. The probability that the next medication will achieve seizure freedom drops with every failed AED. For example, after two failed AEDs, the probability that the third will achieve seizure freedom is around 4%. Drug-resistant epilepsy is commonly diagnosed after several years of uncontrolled seizures, however, in most cases, it is evident much earlier. Approximately 30% of people with epilepsy have a drug-resistant form.
Musicogenic seizure, also known as music-induced seizure, is a rare type of seizure, with an estimated prevalence of 1 in 10,000,000 individuals, that arises from disorganized or abnormal brain electrical activity when a person hears or is exposed to a specific type of sound or musical stimuli. There are challenges when diagnosing a music-induced seizure due to the broad scope of triggers, and time delay between a stimulus and seizure. In addition, the causes of musicogenic seizures are not well-established as solely limited cases and research have been discovered and conducted respectively. Nevertheless, the current understanding of the mechanism behind musicogenic seizure is that music triggers the part of the brain that is responsible for evoking an emotion associated with that music. Dysfunction in this system leads to an abnormal release of dopamine, eventually inducing seizure.