Medical Uses
Non- steroidal Anti- inflammatory drugs (NSAIDs)
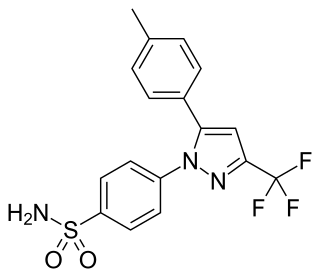
NSAIDs are used as anti- inflammatory, antipyretic and analgesic agents. [4] They can be administered through different routes, namely oral, rectal and topical. [4] They can relieve mild to moderate pain. [5] The dosage forms available for different NSAIDs and their respective medical uses are discussed as follows.
The available dosage forms for oral NSAIDs, rectal NSAIDs and topical NSAIDs are shown in the following table.
| Oral NSAIDs | Rectal NSAIDs | Topical NSAIDs | |
|---|---|---|---|
| Available dosage forms | Tablets and capsules [6] | Suppository [7] | Gels, creams and suppository [8] |
The common medical uses of oral NSAIDs, rectal NSAIDs and topical NSAIDs are shown in the following table.
| Oral NSAIDs | Rectal NSAIDs | Topical NSAIDs | |
|---|---|---|---|
| Medical Uses | 1. Common Cold and Flu Oral NSAIDs are commonly prescribed for relieving the symptoms of common cold and flu. [9] They are shown to be effective to alleviate symptoms such as sneezing, [9] headache, ear pain, muscle pain and malaise. [10] However, studies show that NSAIDs are not effective in treating cough and blocked nose. [10] 2.Postoperative Pain The American Society of Anesthesiologists Task Force on Acute Pain Management recommended the use of oral NSAIDs for managing postoperative pain in 2012. [5] The commonly used NSAIDs for postoperative pain are celecoxib and ibuprofen. [5] Trials have shown that these drugs can reduce pain to at least 50% and they are tolerable by most patients. [5] 3. Migraine The therapeutic goals for migraine treatment are migraine prevention and symptomatic relief. [11] The majority of oral NSAIDs such as ibuprofen, mefenamic acid, and indomethacin are shown to be effective to treat and prevent migraine. [11] They do not have significant differences in terms of their therapeutic effects and are almost equally potent in migraine therapy. [11] NSAIDs with less side effects are more preferred in migraine therapy. [11] | Prevention of pancreatitis Rectal NSAIDs such as diclofenac and indomethacin are administered for the prevention of pancreatitis due to endoscopic retrograde cholangiopancreatography (ERCP). [12] ERCP is a technique for treating liver and pancreatic disease. [7] Acute pancreatitis is the most common complication of ERCP. Therefore, rectal NSAIDs are given to patients before ERCP as a measure to prevent post- ERCP pancreatits. Trials showed that rectal NSAIDs are more effective than oral NSAIDs to prevent post ERCP pancreatitis as it exerts its effects faster and its degree of absorption is higher. [7]  | Osteoarthritis Topical NSAIDs, mainly diclofenac, are prescribed for patients with osteoarthritis. [8] They are effectively absorbed in arms and knees. As osteoarthritis is a disease commonly found in the elderly (>65 years old), oral NSAIDs are seldom used as their systemic side effects are more severe in elderly patients. [8] Therefore, topical NSAIDs are used for osteoarthritis to exert its local analgesic effects and minimize their systemic side effects in elderly patients. [8]  |
Glucocorticoids
Glucocorticoids are potent anti- inflammatory drugs. [10] They are mainly administered via oral and pulmonary route. [10] Oral glucocorticoids are mainly prescribed for the prevention of chronic disease exacerbation. Inhalable glucocorticoids are effective in treating small airways inflammations. [10] They are commonly used in the maintenance of chronic diseases, and to relieve symptoms during acute flare up of airway inflammations such as asthma. [10] The dosage forms available for different glucocorticoids and their medical uses are discussed as follows.
The available dosage forms for oral glucocorticoids and inhalable glucocorticoids are shown in the following table.
| Oral Glucocorticoids | Inhalable Glucocoticoids | |
|---|---|---|
| Available dosage forms | Tablets, capsules and liquid [13] | Dry powder [14] |
The common medical uses of oral glucocorticoids and inhalable glucocorticoids are summarized in the following table.
| Oral Glucocorticoids | Inhalable Glucocorticoids | |
|---|---|---|
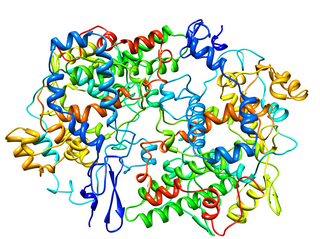
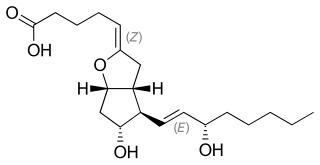
| Medical uses | Rheumatoid arthritis Rheumatoid arthritis is an auto- immune disorder that affect joints. [15] The common symptoms are warm, painful and swollen joints. [15] Glucocorticoids exert anti- inflammatory effects to relieve the symptoms by inhibiting the synthesis of prostaglandin and leukotriene, and the release of collagenase and lysosomal enzymes. [16]  | Asthma Inhalable glucocorticoids are the major drugs used for asthma treatment and maintenance. [13] They suppress airway inflammation in asthma by inhibiting prostaglandin synthesis, enhancing gene expression of anti- inflammatory proteins, and suppressing inflammatory genes. [17] They also dilate airway by reducing the production of leukotriene, a potent bronchoconstrictor in the circulation. [17]  |