Parathyroid hormone (PTH), also called parathormone or parathyrin, is a peptide hormone secreted by the parathyroid glands that regulates the serum calcium concentration through its effects on bone, kidney, and intestine.

Calcium metabolism is the movement and regulation of calcium ions (Ca2+) in (via the gut) and out (via the gut and kidneys) of the body, and between body compartments: the blood plasma, the extracellular and intracellular fluids, and bone. Bone acts as a calcium storage center for deposits and withdrawals as needed by the blood via continual bone remodeling.
Hypercalcemia, also spelled hypercalcaemia, is a high calcium (Ca2+) level in the blood serum. The normal range is 2.1–2.6 mmol/L (8.8–10.7 mg/dL, 4.3–5.2 mEq/L), with levels greater than 2.6 mmol/L defined as hypercalcemia. Those with a mild increase that has developed slowly typically have no symptoms. In those with greater levels or rapid onset, symptoms may include abdominal pain, bone pain, confusion, depression, weakness, kidney stones or an abnormal heart rhythm including cardiac arrest.

Hyperparathyroidism is an increase in parathyroid hormone (PTH) levels in the blood. This occurs from a disorder either within the parathyroid glands or as response to external stimuli.

Chronic kidney disease (CKD) is a type of kidney disease in which a gradual loss of kidney function occurs over a period of months to years. Initially generally no symptoms are seen, but later symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, and confusion. Complications can relate to hormonal dysfunction of the kidneys and include high blood pressure, bone disease, and anemia. Additionally CKD patients have markedly increased cardiovascular complications with increased risks of death and hospitalization.

Hyperphosphatemia is an electrolyte disorder in which there is an elevated level of phosphate in the blood. Most people have no symptoms while others develop calcium deposits in the soft tissue. Often there is also low calcium levels which can result in muscle spasms.

Parathyroidectomy is the surgical removal of one or more of the (usually) four parathyroid glands. This procedure is used to remove an adenoma or hyperplasia of these glands when they are producing excessive parathyroid hormone (PTH): hyperparathyroidism. The glands are usually four in number and located adjacent to the posterior surface of the thyroid gland, but their exact location is variable. When an elevated PTH level is found, a sestamibi scan or an ultrasound may be performed in order to confirm the presence and location of abnormal parathyroid tissue.

Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body's acid-base balance. Metabolic acidosis has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys to excrete excess acids. Metabolic acidosis can lead to acidemia, which is defined as arterial blood pH that is lower than 7.35. Acidemia and acidosis are not mutually exclusive – pH and hydrogen ion concentrations also depend on the coexistence of other acid-base disorders; therefore, pH levels in people with metabolic acidosis can range from low to high.
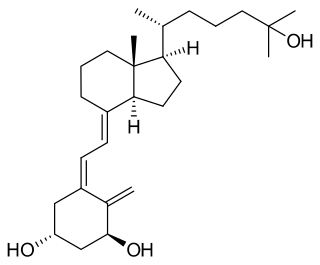
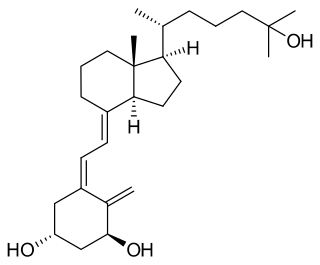
Calcitriol is the active form of vitamin D, normally made in the kidney. It is also known as 1,25-dihydroxycholecalciferol. It is a hormone which binds to and activates the vitamin D receptor in the nucleus of the cell, which then increases the expression of many genes. Calcitriol increases blood calcium (Ca2+) mainly by increasing the uptake of calcium from the intestines.
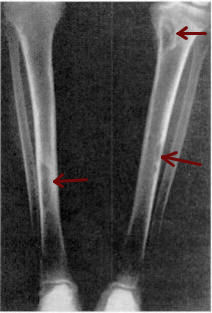
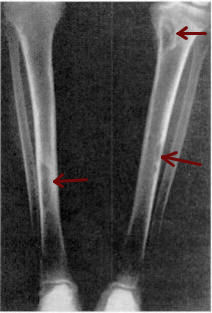
Osteitis fibrosa cystica is a skeletal disorder resulting in a loss of bone mass, a weakening of the bones as their calcified supporting structures are replaced with fibrous tissue, and the formation of cyst-like brown tumors in and around the bone. Osteitis fibrosis cystica (OFC), also known as osteitis fibrosa, osteodystrophia fibrosa, and von Recklinghausen's disease of bone, is caused by hyperparathyroidism, which is a surplus of parathyroid hormone from over-active parathyroid glands. This surplus stimulates the activity of osteoclasts, cells that break down bone, in a process known as osteoclastic bone resorption. The hyperparathyroidism can be triggered by a parathyroid adenoma, hereditary factors, parathyroid carcinoma, or renal osteodystrophy. Osteoclastic bone resorption releases minerals, including calcium, from the bone into the bloodstream, causing both elevated blood calcium levels, and the structural changes which weaken the bone. The symptoms of the disease are the consequences of both the general softening of the bones and the excess calcium in the blood, and include bone fractures, kidney stones, nausea, moth-eaten appearance in the bones, appetite loss, and weight loss.

Secondary hyperparathyroidism is the medical condition of excessive secretion of parathyroid hormone (PTH) by the parathyroid glands in response to hypocalcemia, with resultant hyperplasia of these glands. This disorder is primarily seen in patients with chronic kidney failure. It is sometimes abbreviated "SHPT" in medical literature.

Tertiary hyperparathyroidism is a condition involving the overproduction of the hormone, parathyroid hormone, produced by the parathyroid glands. The parathyroid glands are involved in monitoring and regulating blood calcium levels and respond by either producing or ceasing to produce parathyroid hormone.

Calciphylaxis, also known as calcific uremic arteriolopathy (CUA) or “Grey Scale”, is a rare syndrome characterized by painful skin lesions. The pathogenesis of calciphylaxis is unclear but believed to involve calcification of the small blood vessels located within the fatty tissue and deeper layers of the skin, blood clots, and eventual death of skin cells due to lack of blood flow. It is seen mostly in people with end-stage kidney disease but can occur in the earlier stages of chronic kidney disease and rarely in people with normally functioning kidneys. Calciphylaxis is a rare but serious disease, believed to affect 1-4% of all dialysis patients. It results in chronic non-healing wounds and indicates poor prognosis, with typical life expectancy of less than one year.
Bone disease refers to the medical conditions which affect the bone.

Alfacalcidol is an analogue of vitamin D used for supplementation in humans and as a poultry feed additive.
Calcium acetate/magnesium carbonate is a fixed-dose combination drug that contains 110 mg calcium and 60 mg magnesium ions and is indicated as a phosphate binder for dialysis patients with hyperphosphataemia. It is registered by Fresenius Medical Care under the trade names Renepho (Belgium) and OsvaRen.
Sucroferric oxyhydroxide, sold under the brand name Velphoro, is a non-calcium, iron-based phosphate binder used for the control of serum phosphorus levels in adults with chronic kidney disease (CKD) on haemodialysis (HD) or peritoneal dialysis (PD). It is used in form of chewable tablets.
Chronic kidney disease–mineral and bone disorder (CKD–MBD) is one of the many complications associated with chronic kidney disease. It represents a systemic disorder of mineral and bone metabolism due to CKD manifested by either one or a combination of the following:
A renal diet is a diet aimed at keeping levels of fluids, electrolytes, and minerals balanced in the body in individuals with chronic kidney disease or who are on dialysis. Dietary changes may include the restriction of fluid intake, protein, and electrolytes including sodium, phosphorus, and potassium. Calories may also be supplemented if the individual is losing weight undesirably.

Idiopathic hypercalcinuria (IH) is a condition including an excessive urinary calcium level with a normal blood calcium level resulting from no underlying cause. IH has become the most common cause of hypercalciuria and is the most serious metabolic risk factor for developing nephrolithiasis. IH can predispose individuals to osteopenia or osteoporosis, and affects the entire body. IH arises due to faulty calcium homeostasis, a closely monitored process, where slight deviations in calcium transport in the intestines, blood, and bone can lead to excessive calcium excretion, bone mineral density loss, or kidney stone formation. 50%-60% of nephrolithiasis patients suffer from IH and have 5%-15% lower bone density than those who do not.