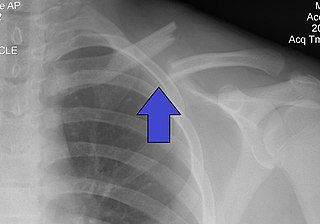
The clavicle, or collarbone, is a slender, S-shaped long bone approximately 6 inches (15 cm) long that serves as a strut between the shoulder blade and the sternum (breastbone). There are two clavicles, one on the left and one on the right. The clavicle is the only long bone in the body that lies horizontally. Together with the shoulder blade, it makes up the shoulder girdle. It is a palpable bone and, in people who have less fat in this region, the location of the bone is clearly visible. It receives its name from Latin clavicula 'little key' because the bone rotates along its axis like a key when the shoulder is abducted. The clavicle is the most commonly fractured bone. It can easily be fractured by impacts to the shoulder from the force of falling on outstretched arms or by a direct hit.
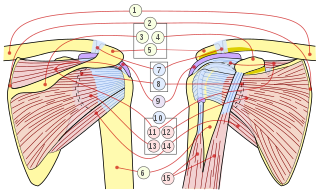
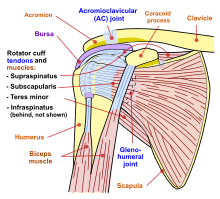
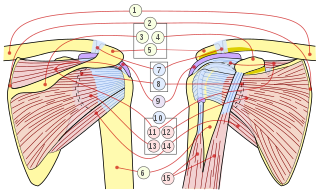
The rotator cuff is a group of muscles and their tendons that act to stabilize the human shoulder and allow for its extensive range of motion. Of the seven scapulohumeral muscles, four make up the rotator cuff. The four muscles are:

The human shoulder is made up of three bones: the clavicle (collarbone), the scapula, and the humerus as well as associated muscles, ligaments and tendons.

The deltoid muscle is the muscle forming the rounded contour of the human shoulder. It is also known as the 'common shoulder muscle', particularly in other animals such as the domestic cat. Anatomically, the deltoid muscle appears to be made up of three distinct sets of muscle fibers, namely the
- anterior or clavicular part
- posterior or scapular part
- intermediate or acromial part
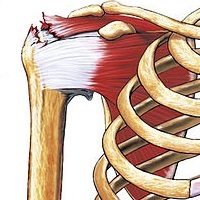
Rotator cuff tendinopathy is a process of senescence. The pathophysiology is mucoid degeneration. Most people develop rotator cuff tendinopathy within their lifetime.
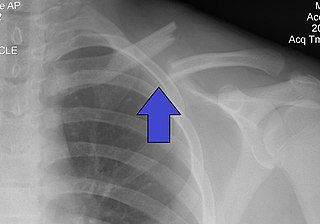
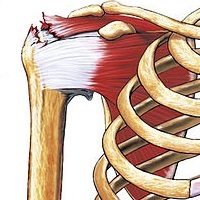
A clavicle fracture, also known as a broken collarbone, is a bone fracture of the clavicle. Symptoms typically include pain at the site of the break and a decreased ability to move the affected arm. Complications can include a collection of air in the pleural space surrounding the lung (pneumothorax), injury to the nerves or blood vessels in the area, and an unpleasant appearance.

The acromioclavicular joint, or AC joint, is a joint at the top of the shoulder. It is the junction between the acromion and the clavicle. It is a plane synovial joint.

The supraspinatus is a relatively small muscle of the upper back that runs from the supraspinous fossa superior portion of the scapula to the greater tubercle of the humerus. It is one of the four rotator cuff muscles and also abducts the arm at the shoulder. The spine of the scapula separates the supraspinatus muscle from the infraspinatus muscle, which originates below the spine.

The shoulder joint is structurally classified as a synovial ball-and-socket joint and functionally as a diarthrosis and multiaxial joint. It involves an articulation between the glenoid fossa of the scapula and the head of the humerus. Due to the very loose joint capsule that gives a limited interface of the humerus and scapula, it is the most mobile joint of the human body.

The shoulder girdle or pectoral girdle is the set of bones in the appendicular skeleton which connects to the arm on each side. In humans it consists of the clavicle and scapula; in those species with three bones in the shoulder, it consists of the clavicle, scapula, and coracoid. Some mammalian species have only the scapula.

The sternoclavicular joint or sternoclavicular articulation is a synovial saddle joint between the manubrium of the sternum, and the clavicle, and the first costal cartilage. The joint possesses a joint capsule, and an articular disc, and is reinforced by multiple ligaments.

The glenoid fossa of the scapula or the glenoid cavity is a bone part of the shoulder. The word glenoid is pronounced or and is from Greek: gléne, "socket", reflecting the shoulder joint's ball-and-socket form. It is a shallow, pyriform articular surface, which is located on the lateral angle of the scapula. It is directed laterally and forward and articulates with the head of the humerus; it is broader below than above and its vertical diameter is the longest.

The coracoacromial ligament is a strong triangular ligament between the coracoid process and the acromion. It protects the head of the humerus. Its acromial attachment may be repositioned to the clavicle during reconstructive surgery of the acromioclavicular joint.

A separated shoulder, also known as acromioclavicular joint injury, is a common injury to the acromioclavicular joint. The AC joint is located at the outer end of the clavicle where it attaches to the acromion of the scapula. Symptoms include non-radiating pain which may make it difficult to move the shoulder. The presence of swelling or bruising and a deformity in the shoulder is also common depending on how severe the dislocation is.

Subacromial bursitis is a condition caused by inflammation of the bursa that separates the superior surface of the supraspinatus tendon from the overlying coraco-acromial ligament, acromion, and coracoid and from the deep surface of the deltoid muscle. The subacromial bursa helps the motion of the supraspinatus tendon of the rotator cuff in activities such as overhead work.

A dislocated shoulder is a condition in which the head of the humerus is detached from the shoulder joint. Symptoms include shoulder pain and instability. Complications may include a Bankart lesion, Hill-Sachs lesion, rotator cuff tear, or injury to the axillary nerve.
Shoulder surgery is a means of treating injured shoulders. Many surgeries have been developed to repair the muscles, connective tissue, or damaged joints that can arise from traumatic or overuse injuries to the shoulder.

Shoulder replacement is a surgical procedure in which all or part of the glenohumeral joint is replaced by a prosthetic implant. Such joint replacement surgery generally is conducted to relieve arthritis pain or fix severe physical joint damage.

The elbow is the region between the upper arm and the forearm that surrounds the elbow joint. The elbow includes prominent landmarks such as the olecranon, the cubital fossa, and the lateral and the medial epicondyles of the humerus. The elbow joint is a hinge joint between the arm and the forearm; more specifically between the humerus in the upper arm and the radius and ulna in the forearm which allows the forearm and hand to be moved towards and away from the body. The term elbow is specifically used for humans and other primates, and in other vertebrates forelimb plus joint is used.

Shoulder impingement syndrome is a syndrome involving tendonitis of the rotator cuff muscles as they pass through the subacromial space, the passage beneath the acromion. It is particularly associated with tendonitis of the supraspinatus muscle. This can result in pain, weakness, and loss of movement at the shoulder.