Serotonin syndrome (SS) is a group of symptoms that may occur with the use of certain serotonergic medications or drugs. The symptoms can range from mild to severe, and are potentially fatal. Symptoms in mild cases include high blood pressure and a fast heart rate; usually without a fever. Symptoms in moderate cases include high body temperature, agitation, increased reflexes, tremor, sweating, dilated pupils, and diarrhea. In severe cases, body temperature can increase to greater than 41.1 °C (106.0 °F). Complications may include seizures and extensive muscle breakdown.
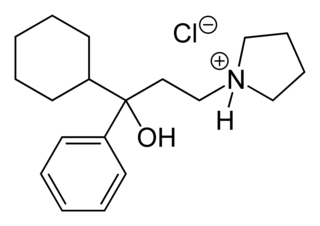
3-Quinuclidinyl benzilate (QNB) is an odorless and bitter-tasting military incapacitating agent. BZ is an antagonist of muscarinic acetylcholine receptors whose structure is the ester of benzilic acid with an alcohol derived from quinuclidine.

Eclampsia is the onset of seizures (convulsions) in a woman with pre-eclampsia. Pre-eclampsia is a hypertensive disorder of pregnancy that presents with three main features: new onset of high blood pressure, large amounts of protein in the urine or other organ dysfunction, and edema. If left untreated, pre-eclampsia can result in long-term consequences for the mother, namely increased risk of cardiovascular diseases and associated complications. In more severe cases, it may be fatal for both the mother and the fetus.

A drug overdose is the ingestion or application of a drug or other substance in quantities much greater than are recommended. Typically it is used for cases when a risk to health will potentially result. An overdose may result in a toxic state or death.
Colloquially known as "downers", depressants or CNS depressants are drugs that lower neurotransmission levels, decrease the electrical activity of brain cells, or reduce arousal or stimulation in various areas of the brain. Some specific depressants do influence mood, either positively or negatively, but depressants often have no clear impact on mood. In contrast, stimulants, or "uppers", increase mental alertness, making stimulants the opposite drug class from depressants. Antidepressants are defined by their effect on mood, not on general brain activity, so they form an orthogonal category of drugs.

Cyclopentolate is a muscarinic antagonist. It is commonly used as an eye drop during pediatric eye examinations to dilate the eye (mydriatic) and prevent the eye from focusing/accommodating (cycloplegic). Cyclopentolate or atropine can also be administered to reverse muscarinic and central nervous system effects of indirect cholinomimetic (anti-AChase) administration.
Anticholinergics are substances that block the action of the acetylcholine (ACh) neurotransmitter at synapses in the central and peripheral nervous system.

Nicotine poisoning describes the symptoms of the toxic effects of nicotine following ingestion, inhalation, or skin contact. Nicotine poisoning can potentially be deadly, though serious or fatal overdoses are rare. Historically, most cases of nicotine poisoning have been the result of use of nicotine as an insecticide. More recent cases of poisoning typically appear to be in the form of Green Tobacco Sickness, or due to unintended ingestion of tobacco or tobacco products or consumption of nicotine-containing plants.

Biperiden, sold under the brand name Akineton among others, is a medication used to treat Parkinson disease, certain drug-induced movement disorders and Tourette Syndrome. It is not recommended for tardive dyskinesias. It is taken by mouth, injection into a vein, or muscle.

Trihexyphenidyl is an antispasmodic drug used to treat stiffness, tremors, spasms, and poor muscle control. It is an agent of the antimuscarinic class and is often used in management of Parkinson's disease. It was approved by the FDA for the treatment of Parkinson's in the US in 2003.
Autonomic dysreflexia (AD) is a potentially fatal medical emergency classically characterized by uncontrolled hypertension and cardiac arrhythmia. AD occurs most often in individuals with spinal cord injuries with lesions at or above the T6 spinal cord level, although it has been reported in patients with lesions as low as T10. Guillain–Barré syndrome may also cause autonomic dysreflexia.
Procyclidine is an anticholinergic drug principally used for the treatment of drug-induced parkinsonism, akathisia and acute dystonia, Parkinson's disease, and idiopathic or secondary dystonia.

Posterior reversible encephalopathy syndrome (PRES), also known as reversible posterior leukoencephalopathy syndrome (RPLS), is a rare condition in which parts of the brain are affected by swelling, usually as a result of an underlying cause. Someone with PRES may experience headaches, changes in vision, and seizures, with some developing other neurological symptoms such as confusion or weakness of one or more limbs. The name of the condition includes the word "posterior" because it predominantly though not exclusively affects the back of the brain. Common underlying causes are severely elevated blood pressure, kidney failure, severe infections, certain medications, some autoimmune diseases, and pre-eclampsia. The diagnosis is usually made by a brain scan (MRI) on which areas of swelling can be identified.

Alcohol withdrawal syndrome (AWS) is a set of symptoms that can occur following a reduction in alcohol use after a period of excessive use. Symptoms typically include anxiety, shakiness, sweating, vomiting, fast heart rate, and a mild fever. More severe symptoms may include seizures, and delirium tremens (DTs); which can be fatal in untreated patients. Symptoms start at around 6 hours after last drink. Peak incidence of seizures occurs at 24-36 hours and peak incidence of delirium tremens is at 48-72 hours.

Tricyclic antidepressant overdose is poisoning caused by excessive medication of the tricyclic antidepressant (TCA) type. Symptoms may include elevated body temperature, blurred vision, dilated pupils, sleepiness, confusion, seizures, rapid heart rate, and cardiac arrest. If symptoms have not occurred within six hours of exposure they are unlikely to occur.

Benzodiazepine overdose describes the ingestion of one of the drugs in the benzodiazepine class in quantities greater than are recommended or generally practiced. The most common symptoms of overdose include central nervous system (CNS) depression, impaired balance, ataxia, and slurred speech. Severe symptoms include coma and respiratory depression. Supportive care is the mainstay of treatment of benzodiazepine overdose. There is an antidote, flumazenil, but its use is controversial.

A coma cocktail is a combination of substances administered in an emergency to comatose individuals when the cause of the coma has not yet been determined. The intention is to work against various causes of a coma seen in an emergency setting including drug overdoses and hypoglycemia. The coma cocktail is sometimes colloquially referred to as a “party pack” by professionals in the pre-hospital emergency medical services field.

Arrhythmias, also known as cardiac arrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia, and a resting heart rate that is too slow – below 60 beats per minute – is called bradycardia. Some types of arrhythmias have no symptoms. Symptoms, when present, may include palpitations or feeling a pause between heartbeats. In more serious cases, there may be lightheadedness, passing out, shortness of breath, chest pain, or decreased level of consciousness. While most cases of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in sudden death.

Amitriptyline/perphenazine is a formulation that contains the tricyclic antidepressant amitriptyline and the medium-potency typical (first-generation) antipsychotic, perphenazine. In the United States amitriptyline/perphenazine is marketed by Mylan Pharmaceuticals Inc. and Remedy Repack Inc.

Cholinergic blocking drugs are a group of drugs that block the action of acetylcholine (ACh), a neurotransmitter, in synapses of the cholinergic nervous system. They block acetylcholine from binding to cholinergic receptors, namely the nicotinic and muscarinic receptors.