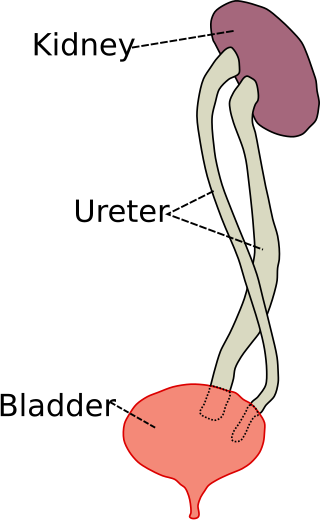
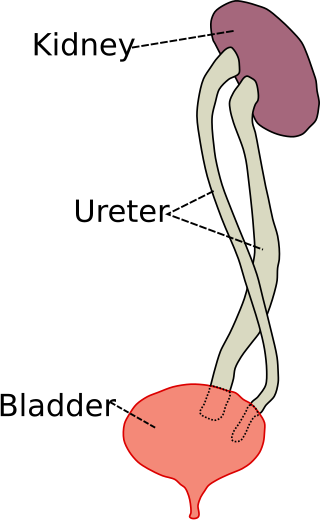
In humans, the kidneys are two reddish-brown bean-shaped blood-filtering organs that are a multilobar, multipapillary form of mammalian kidneys, usually without signs of external lobulation. They are located on the left and right in the retroperitoneal space, and in adult humans are about 12 centimetres in length. They receive blood from the paired renal arteries; blood exits into the paired renal veins. Each kidney is attached to a ureter, a tube that carries excreted urine to the bladder.

The bladder is a hollow organ in humans and other vertebrates that stores urine from the kidneys. In placental mammals, urine enters the bladder via the ureters and exits via the urethra during urination. In humans, the bladder is a distensible organ that sits on the pelvic floor. The typical adult human bladder will hold between 300 and 500 ml before the urge to empty occurs, but can hold considerably more.
Azotemia, also spelled azotaemia, is a medical condition characterized by abnormally high levels of nitrogen-containing compounds in the blood. It is largely related to insufficient or dysfunctional filtering of blood by the kidneys. It can lead to uremia and acute kidney injury if not controlled.
The excretory system is a passive biological system that removes excess, unnecessary materials from the body fluids of an organism, so as to help maintain internal chemical homeostasis and prevent damage to the body. The dual function of excretory systems is the elimination of the waste products of metabolism and to drain the body of used up and broken down components in a liquid and gaseous state. In humans and other amniotes, most of these substances leave the body as urine and to some degree exhalation, mammals also expel them through sweating.

The ureters are tubes composed of smooth muscle that transport urine from the kidneys to the urinary bladder. In an adult human, the ureters typically measure 20 to 30 centimeters in length and about 3 to 4 millimeters in diameter. They are lined with urothelial cells, a form of transitional epithelium, and feature an extra layer of smooth muscle in the lower third to aid in peristalsis. The ureters can be affected by a number of diseases, including urinary tract infections and kidney stone. Stenosis is when a ureter is narrowed, due to for example chronic inflammation. Congenital abnormalities that affect the ureters can include the development of two ureters on the same side or abnormally placed ureters. Additionally, reflux of urine from the bladder back up the ureters is a condition commonly seen in children.
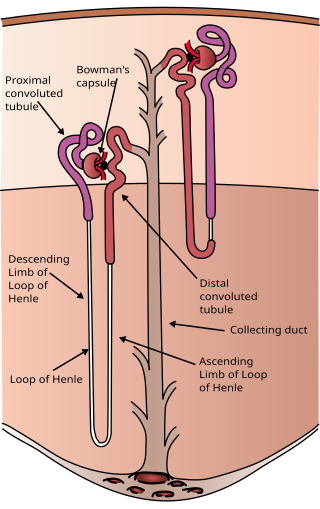
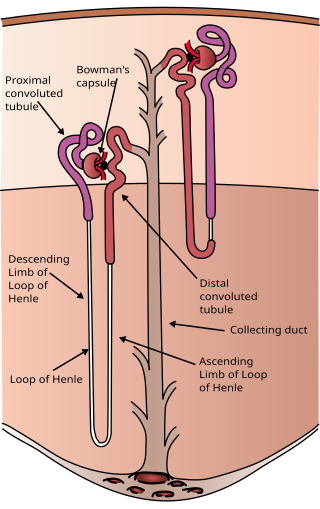
The nephron is the minute or microscopic structural and functional unit of the kidney. It is composed of a renal corpuscle and a renal tubule. The renal corpuscle consists of a tuft of capillaries called a glomerulus and a cup-shaped structure called Bowman's capsule. The renal tubule extends from the capsule. The capsule and tubule are connected and are composed of epithelial cells with a lumen. A healthy adult has 1 to 1.5 million nephrons in each kidney. Blood is filtered as it passes through three layers: the endothelial cells of the capillary wall, its basement membrane, and between the podocyte foot processes of the lining of the capsule. The tubule has adjacent peritubular capillaries that run between the descending and ascending portions of the tubule. As the fluid from the capsule flows down into the tubule, it is processed by the epithelial cells lining the tubule: water is reabsorbed and substances are exchanged ; first with the interstitial fluid outside the tubules, and then into the plasma in the adjacent peritubular capillaries through the endothelial cells lining that capillary. This process regulates the volume of body fluid as well as levels of many body substances. At the end of the tubule, the remaining fluid—urine—exits: it is composed of water, metabolic waste, and toxins.

The collecting duct system of the kidney consists of a series of tubules and ducts that physically connect nephrons to a minor calyx or directly to the renal pelvis. The collecting duct participates in electrolyte and fluid balance through reabsorption and excretion, processes regulated by the hormones aldosterone and vasopressin.

Renal physiology is the study of the physiology of the kidney. This encompasses all functions of the kidney, including maintenance of acid-base balance; regulation of fluid balance; regulation of sodium, potassium, and other electrolytes; clearance of toxins; absorption of glucose, amino acids, and other small molecules; regulation of blood pressure; production of various hormones, such as erythropoietin; and activation of vitamin D.

Hematuria or haematuria is defined as the presence of blood or red blood cells in the urine. "Gross hematuria" occurs when urine appears red, brown, or tea-colored due to the presence of blood. Hematuria may also be subtle and only detectable with a microscope or laboratory test. Blood that enters and mixes with the urine can come from any location within the urinary system, including the kidney, ureter, urinary bladder, urethra, and in men, the prostate. Common causes of hematuria include urinary tract infection (UTI), kidney stones, viral illness, trauma, bladder cancer, and exercise. These causes are grouped into glomerular and non-glomerular causes, depending on the involvement of the glomerulus of the kidney. But not all red urine is hematuria. Other substances such as certain medications and foods can cause urine to appear red. Menstruation in women may also cause the appearance of hematuria and may result in a positive urine dipstick test for hematuria. A urine dipstick test may also give an incorrect positive result for hematuria if there are other substances in the urine such as myoglobin, a protein excreted into urine during rhabdomyolysis. A positive urine dipstick test should be confirmed with microscopy, where hematuria is defined by three or more red blood cells per high power field. When hematuria is detected, a thorough history and physical examination with appropriate further evaluation can help determine the underlying cause.
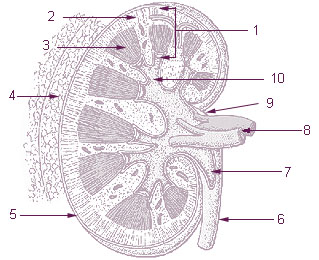
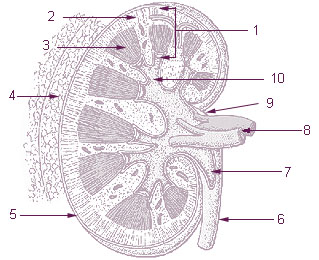
The renal medulla is the innermost part of the kidney. The renal medulla is split up into a number of sections, known as the renal pyramids. Blood enters into the kidney via the renal artery, which then splits up to form the segmental arteries which then branch to form interlobar arteries. The interlobar arteries each in turn branch into arcuate arteries, which in turn branch to form interlobular arteries, and these finally reach the glomeruli. At the glomerulus the blood reaches a highly disfavourable pressure gradient and a large exchange surface area, which forces the serum portion of the blood out of the vessel and into the renal tubules. Flow continues through the renal tubules, including the proximal tubule, the loop of Henle, through the distal tubule and finally leaves the kidney by means of the collecting duct, leading to the renal pelvis, the dilated portion of the ureter.

Hydronephrosis describes hydrostatic dilation of the renal pelvis and calyces as a result of obstruction to urine flow downstream. Alternatively, hydroureter describes the dilation of the ureter, and hydronephroureter describes the dilation of the entire upper urinary tract.
Kidney development, or nephrogenesis, describes the embryologic origins of the kidney, a major organ in the urinary system. This article covers a 3 part developmental process that is observed in most reptiles, birds and mammals, including humans. Nephrogenesis is often considered in the broader context of the development of the urinary and reproductive organs.

A ureteral stent, or ureteric stent, is a thin tube inserted into the ureter to prevent or treat obstruction of the urine flow from the kidney. The length of the stents used in adult patients varies between 24 and 30 cm. Additionally, stents come in differing diameters or gauges, to fit different size ureters. The stent is usually inserted with the aid of a cystoscope. One or both ends of the stent may be coiled to prevent it from moving out of place; this is called a JJ stent, double J stent or pig-tail stent.
Pyelogram is a form of imaging of the renal pelvis and ureter.
Urologic diseases or conditions include urinary tract infections, kidney stones, bladder control problems, and prostate problems, among others. Some urologic conditions do not affect a person for that long and some are lifetime conditions. Kidney diseases are normally investigated and treated by nephrologists, while the specialty of urology deals with problems in the other organs. Gynecologists may deal with problems of incontinence in women.
Bladder outlet obstruction occurs when urine is unable to flow from the kidneys through the ureters and out of the bladder through the urethra. Decreased flow of urine leads to swelling of the urinary tract, called hydronephrosis. This process of decreased flow of urine through the urinary tract can begin as early as during intrauterine life and it prevents normal development of fetal kidneys and fetal urine. Low levels of fetal urine leads to low amniotic fluid levels and incomplete lung maturation. Older children and adults can also experience bladder outlet obstruction; however, this process is usually reversible and isn't associated with as many poor outcomes as in infants with congenital bladder outlet obstruction.
Duplicated ureter or duplex collecting system is a congenital condition in which the ureteric bud, the embryological origin of the ureter, splits, resulting in two ureters draining a single kidney. It is the most common renal abnormality, occurring in approximately 1% of the population.
The rock dove, Columbia livia, has a number of special adaptations for regulating water uptake and loss.
The kidneys are a pair of organs of the excretory system in vertebrates, which maintain the balance of water and electrolytes in the body (osmoregulation), filter the blood, remove metabolic waste products, and, in many vertebrates, also produce hormones and maintain blood pressure. In healthy vertebrates, the kidneys maintain homeostasis of extracellular fluid in the body. When the blood is being filtered, the kidneys form urine, which consists of water and excess or unnecessary substances, the urine is then excreted from the body through other organs, which in vertebrates, depending on the species, may include the ureter, urinary bladder, cloaca, and urethra.

The mammalian kidneys are a pair of excretory organs of the urinary system of mammals, being functioning kidneys in postnatal-to-adult individuals. The kidneys in mammals are usually bean-shaped or externally lobulated. They are located behind the peritoneum (retroperitoneally) on the back (dorsal) wall of the body. The typical mammalian kidney consists of a renal capsule, a peripheral cortex, an internal medulla, one or more renal calyces, and a renal pelvis. Although the calyces or renal pelvis may be absent in some species. The medulla is made up of one or more renal pyramids, forming papillae with their innermost parts. Generally, urine produced by the cortex and medulla drains from the papillae into the calyces, and then into the renal pelvis, from which urine exits the kidney through the ureter. Nitrogen-containing waste products are excreted by the kidneys in mammals mainly in the form of urea.