The perineum in mammals is the space between the anus and the genitals. The human perineum is between the anus and scrotum in the male or between the anus and vulva in the female. The perineum is the region of the body between the pubic symphysis and the coccyx, including the perineal body and surrounding structures. The perineal raphe is visible and pronounced to varying degrees. The perineum is an erogenous zone. This area is also known as the taint or gooch in American slang.
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. It has been identified as an important issue in geriatric health care. The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis. UI is an example of a stigmatized medical condition, which creates barriers to successful management and makes the problem worse. People may be too embarrassed to seek medical help, and attempt to self-manage the symptom in secrecy from others.

The levator ani is a broad, thin muscle group, situated on either side of the pelvis. It is formed from three muscle components: the pubococcygeus, the iliococcygeus, and the puborectalis.

Kegel exercise, also known as pelvic floor exercise, involves repeatedly contracting and relaxing the muscles that form part of the pelvic floor, now sometimes colloquially referred to as the "Kegel muscles". The exercise can be performed many times a day, for several minutes at a time but takes one to three months to begin to have an effect.
A pessary is a prosthetic device inserted into the vagina for structural and pharmaceutical purposes. It is most commonly used to treat stress urinary incontinence to stop urinary leakage and to treat pelvic organ prolapse to maintain the location of organs in the pelvic region. It can also be used to administer medications locally in the vagina or as a method of contraception.

Pelvic floor dysfunction is a term used for a variety of disorders that occur when pelvic floor muscles and ligaments are impaired. The condition affects up to 50 percent of women who have given birth. Although this condition predominantly affects women, up to 16 percent of men are affected as well. Symptoms can include pelvic pain, pressure, pain during sex, urinary incontinence (UI), overactive bladder, bowel incontinence, incomplete emptying of feces, constipation, myofascial pelvic pain and pelvic organ prolapse. When pelvic organ prolapse occurs, there may be visible organ protrusion or a lump felt in the vagina or anus. Research carried out in the UK has shown that symptoms can restrict everyday life for women. However, many people found it difficult to talk about it and to seek care, as they experienced embarrassment and stigma.

Older texts have asserted the existence of a urogenital diaphragm, also called the triangular ligament, which was described as a layer of the pelvis that separates the deep perineal sac from the upper pelvis, lying between the inferior fascia of the urogenital diaphragm and superior fascia of the urogenital diaphragm.

The cystocele, also known as a prolapsed bladder, is a medical condition in which a woman's bladder bulges into her vagina. Some may have no symptoms. Others may have trouble starting urination, urinary incontinence, or frequent urination. Complications may include recurrent urinary tract infections and urinary retention. Cystocele and a prolapsed urethra often occur together and is called a cystourethrocele. Cystocele can negatively affect quality of life.

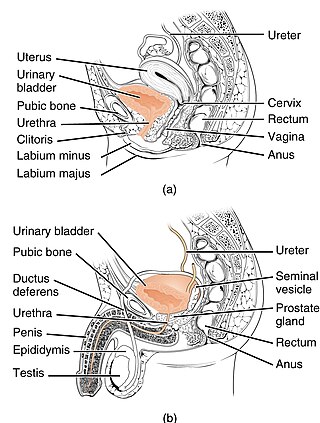
Prostatectomy is the surgical removal of all or part of the prostate gland. This operation is done for benign conditions that cause urinary retention, as well as for prostate cancer and for other cancers of the pelvis.

Pelvic organ prolapse (POP) is characterized by descent of pelvic organs from their normal positions into the vagina. In women, the condition usually occurs when the pelvic floor collapses after gynecological cancer treatment, childbirth or heavy lifting. Injury incurred to fascia membranes and other connective structures can result in cystocele, rectocele or both. Treatment can involve dietary and lifestyle changes, physical therapy, or surgery.

Stress incontinence, also known as stress urinary incontinence (SUI) or effort incontinence is a form of urinary incontinence. It is due to inadequate closure of the bladder outlet by the urethral sphincter.

The deep perineal pouch is the anatomic space enclosed in part by the perineum and located superior to the perineal membrane.

The urethral sphincters are two muscles used to control the exit of urine in the urinary bladder through the urethra. The two muscles are either the male or female external urethral sphincter and the internal urethral sphincter. When either of these muscles contracts, the urethra is sealed shut.

Defecography is a type of medical radiological imaging in which the mechanics of a patient's defecation are visualized in real time using a fluoroscope. The anatomy and function of the anorectum and pelvic floor can be dynamically studied at various stages during defecation.
Urogynecology or urogynaecology is a surgical sub-specialty of urology and gynecology.
Descending perineum syndrome refers to a condition where the perineum "balloons" several centimeters below the bony outlet of the pelvis during strain, although this descent may happen without straining. The syndrome was first described in 1966 by Parks et al.
Urethral hypermobility is a condition of excessive movement of the female urethra due to a weakened urogenital diaphragm. It describes the instability of the urethra in relation to the pelvic floor muscles. A weakened pelvic floor muscle fails to adequately close the urethra and hence can cause stress urinary incontinence. This condition may be diagnosed by primary care providers or urologists. Treatment may include pelvic floor muscle exercises, surgery, or minimally invasive procedures.

The vaginal support structures are those muscles, bones, ligaments, tendons, membranes and fascia, of the pelvic floor that maintain the position of the vagina within the pelvic cavity and allow the normal functioning of the vagina and other reproductive structures in the female. Defects or injuries to these support structures in the pelvic floor leads to pelvic organ prolapse. Anatomical and congenital variations of vaginal support structures can predispose a woman to further dysfunction and prolapse later in life. The urethra is part of the anterior wall of the vagina and damage to the support structures there can lead to incontinence and urinary retention.
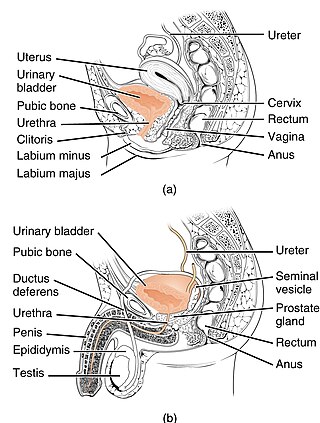
The urogenital hiatus is a gap in the anteromedial part of the pelvic floor, allowing passage of the urethra, the vagina, and deep dorsal vein of clitoris (females) or penis (males).
Transvaginal mesh, also known as vaginal mesh implant, is a net-like surgical tool that is used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI) among female patients. The surgical mesh is placed transvaginally to reconstruct weakened pelvic muscle walls and to support the urethra or bladder.