Related Research Articles

Asthma is a long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wheezing, coughing, chest tightness, and shortness of breath. These may occur a few times a day or a few times per week. Depending on the person, asthma symptoms may become worse at night or with exercise.

A cough is a sudden expulsion of air through the large breathing passages which can help clear them of fluids, irritants, foreign particles and microbes. As a protective reflex, coughing can be repetitive with the cough reflex following three phases: an inhalation, a forced exhalation against a closed glottis, and a violent release of air from the lungs following opening of the glottis, usually accompanied by a distinctive sound.
Shortness of breath (SOB), also medically known as dyspnea or dyspnoea, is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity", and recommends evaluating dyspnea by assessing the intensity of its distinct sensations, the degree of distress and discomfort involved, and its burden or impact on the patient's activities of daily living. Distinct sensations include effort/work to breathe, chest tightness or pain, and "air hunger". The tripod position is often assumed to be a sign.

Pulmonary heart disease, also known as cor pulmonale, is the enlargement and failure of the right ventricle of the heart as a response to increased vascular resistance or high blood pressure in the lungs.
Bronchiolitis is inflammation of the small airways in the lungs. Acute bronchiolitis is due to a viral infection usually affecting children younger than two years of age. Symptoms may include fever, cough, runny nose, wheezing, and breathing problems. More severe cases may be associated with nasal flaring, grunting, or the skin between the ribs pulling in with breathing. If the child has not been able to feed properly, signs of dehydration may be present.
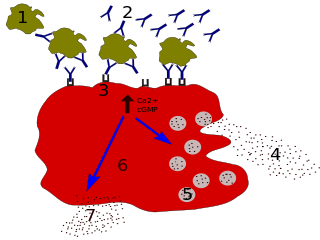
Immunoglobulin E (IgE) is a type of antibody that has been found only in mammals. IgE is synthesised by plasma cells. Monomers of IgE consist of two heavy chains and two light chains, with the ε chain containing four Ig-like constant domains (Cε1–Cε4). IgE is thought to be an important part of the immune response against infection by certain parasitic worms, including Schistosoma mansoni, Trichinella spiralis, and Fasciola hepatica. IgE is also utilized during immune defense against certain protozoan parasites such as Plasmodium falciparum. IgE may have evolved as a defense to protect against venoms.

Bronchospasm or a bronchial spasm is a sudden constriction of the muscles in the walls of the bronchioles. It is caused by the release (degranulation) of substances from mast cells or basophils under the influence of anaphylatoxins. It causes difficulty in breathing which ranges from mild to severe.

Bronchoconstriction is the constriction of the airways in the lungs due to the tightening of surrounding smooth muscle, with consequent coughing, wheezing, and shortness of breath.

Pneumonitis describes general inflammation of lung tissue. Possible causative agents include radiation therapy of the chest, exposure to medications used during chemo-therapy, the inhalation of debris, aspiration, herbicides or fluorocarbons and some systemic diseases. If unresolved, continued inflammation can result in irreparable damage such as pulmonary fibrosis.
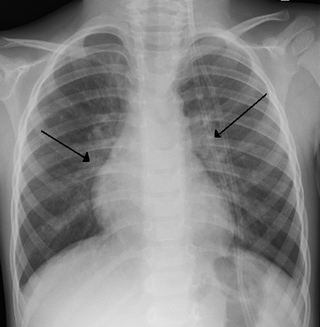
Eosinophilic pneumonia is a disease in which an eosinophil, a type of white blood cell, accumulates in the lungs. These cells cause disruption of the normal air spaces (alveoli) where oxygen is extracted from the atmosphere. Several different kinds of eosinophilic pneumonia exist and can occur in any age group. The most common symptoms include cough, fever, difficulty breathing, and sweating at night. Eosinophilic pneumonia is diagnosed by a combination of characteristic symptoms, findings on a physical examination by a health provider, and the results of blood tests and X-rays. Prognosis is excellent once most eosinophilic pneumonia is recognized and treatment with corticosteroids is begun.
Exercise-induced asthma (EIA) occurs when the airways narrow as a result of exercise. The preferred term for this condition is exercise-induced bronchoconstriction (EIB). While exercise does not cause asthma, it is frequently an asthma trigger.
Feline asthma is a common allergic respiratory disease in cats, affecting at least one percent of all adult cats worldwide. It is a chronic progressive disease for which there is no cure. Common symptoms include wheezing, coughing, labored breathing and potentially life-threatening bronchoconstriction. There is conjecture that the disease has become more common due to increased exposure to industrial pollutants. Feline asthma can also be attributed to lung damage caused by long-term exposure to second-hand smoke.
Allergic bronchopulmonary aspergillosis (ABPA) is a condition characterised by an exaggerated response of the immune system to the fungus Aspergillus. It occurs most often in people with asthma or cystic fibrosis. Aspergillus spores are ubiquitous in soil and are commonly found in the sputum of healthy individuals. A. fumigatus is responsible for a spectrum of lung diseases known as aspergilloses.
Recurrent airway obstruction, also known as broken wind, heaves, wind-broke horse, or sometimes by the term usually reserved for humans, chronic obstructive pulmonary disease or disorder (COPD) – it is a respiratory disease or chronic condition of horses involving an allergic bronchitis characterised by wheezing, coughing and laboured breathing.

Obstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself. It is generally characterized by inflamed and easily collapsible airways, obstruction to airflow, problems exhaling, and frequent medical clinic visits and hospitalizations. Types of obstructive lung disease include; asthma, bronchiectasis, bronchitis and chronic obstructive pulmonary disease (COPD). Although COPD shares similar characteristics with all other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms, and reversibility of airway obstruction. Cystic fibrosis is also sometimes included in obstructive pulmonary disease.
Vocal cord dysfunction (VCD) is a pathology affecting the vocal folds characterized by full or partial vocal fold closure causing difficulty and distress during respiration, especially during inhalation.

An acute exacerbation of chronic obstructive pulmonary disease, or acute exacerbations of chronic bronchitis (AECB), is a sudden worsening of chronic obstructive pulmonary disease (COPD) symptoms including shortness of breath, quantity and color of phlegm that typically lasts for several days.

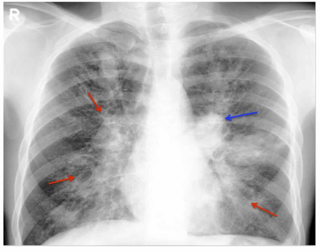
Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. The main symptoms of COPD include shortness of breath and a cough, which may or may not produce mucus. COPD progressively worsens, with everyday activities such as walking or dressing becoming difficult. While COPD is incurable, it is preventable and treatable. The two most common types of COPD are emphysema and chronic bronchitis and have been the two classic COPD phenotypes. Emphysema is defined as enlarged airspaces (alveoli) whose walls have broken down resulting in permanent damage to the lung tissue. Chronic bronchitis is defined as a productive cough that is present for at least three months each year for two years. Both of these conditions can exist without airflow limitation when they are not classed as COPD. Emphysema is just one of the structural abnormalities that can limit airflow and can exist without airflow limitation in a significant number of people. Chronic bronchitis does not always result in airflow limitation but in young adults who smoke the risk of developing COPD is high. Many definitions of COPD in the past included emphysema and chronic bronchitis, but these have never been included in GOLD report definitions. Emphysema and chronic bronchitis remain the predominant phenotypes of COPD but there is often overlap between them and a number of other phenotypes have also been described. COPD and asthma may coexist and converge in some individuals. COPD is associated with low-grade systemic inflammation.
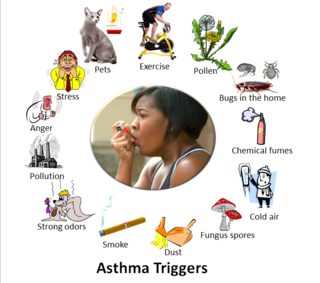
Asthma triggers are factors or stimuli that provoke the exacerbation of asthma symptoms or increase the degree of airflow disruption, which can lead to an asthma attack. An asthma attack is characterized by an obstruction of the airway, hypersecretion of mucus and bronchoconstriction due to the contraction of smooth muscles around the respiratory tract. Its symptoms include a wide range of manifestations such as breathlessness, coughing, a tight chest and wheezing.
Asthma-Chronic Obstructive Pulmonary Disease (COPD) Overlap (ACO), also known as Asthma-COPD Overlap Syndrome (ACOS) is a chronic inflammatory, obstructive airway disease in which features of both asthma and COPD predominate. Asthma and COPD were once thought of as distinct entities, however in some, there are clinical features of both asthma and COPD with significant overlap in pathophysiology and symptom profile. It is unclear whether ACO is a separate disease entity or a clinical subtype of asthma and COPD. The pathogenesis of ACO is poorly understood, but it is thought to involve both type 2 inflammation as well as type 1 inflammation. The incidence and prevalence of ACO are not well known. The risk factors for ACO are also incompletely understood, but tobacco smoke is known to be a major risk factor.
References
- 1 2 "What Is an Asthma Attack?". WebMD. 2019-01-30. Retrieved 2020-03-24.
- ↑ Shah, Rachna; Saltoun, Carol A. (May–June 2012). "Chapter 14: Acute severe asthma (status asthmaticus)". Allergy and Asthma Proceedings. 33 Suppl 1 (3): 47–50. doi:10.2500/aap.2012.33.3547. PMID 22794687 . Retrieved 2019-11-06.
- ↑ "Asthma". The Lecturio Medical Concept Library. 25 November 2020. Retrieved 1 July 2021.
- 1 2 Cheung, Dorothy S.; Ehlenbach, Sarah J.; Kitchens, Robert T.; Riley, Desiré A.; Thomas, Larry L.; Holtzman, Michael J.; Grayson, Mitchell H. (2010-11-01). "CD49d+ neutrophils induce FcεRI expression on lung dendritic cells in a mouse model of postviral asthma". Journal of Immunology. 185 (9): 4983–4987. doi:10.4049/jimmunol.1002456. ISSN 0022-1767. PMC 2959147 . PMID 20876348.
- ↑ Kumar, Varun (2020-10-15). "Asthma". Bibo. Retrieved 2020-11-04.
- 1 2 3 4 "SIGN 141 • British guideline on the management of asthma". Clinical guideline: asthma. London: British Thoracic Society and Scottish Intercollegiate Guidelines Network (BTS/SIGN). October 2014. Archived from the original on 12 September 2017. Retrieved 19 October 2014.
- 1 2 "Status Asthmaticus (Severe Acute Asthma)". WebMD. Retrieved 2019-11-06.
- ↑ Ratto, David; Alfaro, Carlos; Sipsey, Jeff; Glovsky, M. Michael; Sharma, Om P. (1988-07-22). "Are Intravenous Corticosteroids Required in Status Asthmaticus?". JAMA. 260 (4): 527–529. doi:10.1001/jama.1988.03410040099036. ISSN 0098-7484. PMID 3385910.
- ↑ Jat, KanaRam; Tiwari, Abhimanyu; Guglani, Vishal (2016). "Ketamine versus aminophylline for acute asthma in children: A randomized, controlled trial". Annals of Thoracic Medicine. 11 (4): 283–288. doi: 10.4103/1817-1737.191874 . ISSN 1817-1737. PMC 5070438 . PMID 27803755.
- ↑ Holtzman, Michael J.; Patel, Dhara; Zhang, Yong; Patel, Anand C. (August 2011). "Host epithelial-viral interactions as cause and cure for asthma". Current Opinion in Immunology. 23 (4): 487–494. doi:10.1016/j.coi.2011.05.010. ISSN 0952-7915. PMC 3163712 . PMID 21703838.
- ↑ Moore PE, Ryckman KK, Williams SM, Patel N, Summar ML, Sheller JR (9 July 2009). "Genetic variants of GSNOR and ADRB2 influence response to albuterol in African-American children with severe asthma". Pediatric Pulmonology. 44 (7): 649–654. doi:10.1002/ppul.21033. PMID 19514054. S2CID 30530302.