The cervix or cervix uteri is the lower part of the uterus (womb) in the human female reproductive system. The cervix is usually 2 to 3 cm long and roughly cylindrical in shape, which changes during pregnancy. The narrow, central cervical canal runs along its entire length, connecting the uterine cavity and the lumen of the vagina. The opening into the uterus is called the internal os, and the opening into the vagina is called the external os. The lower part of the cervix, known as the vaginal portion of the cervix, bulges into the top of the vagina. The cervix has been documented anatomically since at least the time of Hippocrates, over 2,000 years ago.
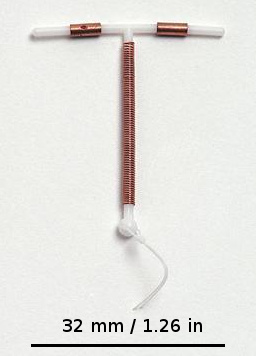
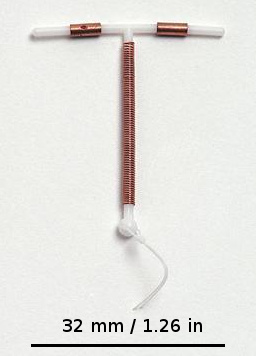
A copper intrauterine device (IUD), also known as an intrauterine coil or copper coil or non-hormonal IUD, is a type of intrauterine device which contains copper. It is used for birth control and emergency contraception within five days of unprotected sex. It is one of the most effective forms of birth control with a one-year failure rate around 0.7%. The device is placed in the uterus and lasts up to twelve years. It may be used by women of all ages regardless of whether or not they have had children. Following removal, fertility quickly returns.

Fertility awareness (FA) refers to a set of practices used to determine the fertile and infertile phases of a woman's menstrual cycle. Fertility awareness methods may be used to avoid pregnancy, to achieve pregnancy, or as a way to monitor gynecological health.

Safe sex is sexual activity using methods or contraceptive devices to reduce the risk of transmitting or acquiring sexually transmitted infections (STIs), especially HIV. "Safe sex" is also sometimes referred to as safer sex or protected sex to indicate that some safe sex practices do not eliminate STI risks. It is also sometimes used colloquially to describe methods aimed at preventing pregnancy that may or may not also lower STI risks.

The diaphragm is a barrier method of birth control. It is moderately effective, with a one-year failure rate of around 12% with typical use. It is placed over the cervix with spermicide before sex and left in place for at least six hours after sex. Fitting by a healthcare provider is generally required.

Nonoxynol-9, sometimes abbreviated as N-9, is an organic compound that is used as a surfactant. It is a member of the nonoxynol family of nonionic surfactants. N-9 and related compounds are ingredients in various cleaning and cosmetic products. It is widely used in contraceptives for its spermicidal properties.
Spermicide is a contraceptive substance that destroys sperm, inserted vaginally prior to intercourse to prevent pregnancy. As a contraceptive, spermicide may be used alone. However, the pregnancy rate experienced by couples using only spermicide is higher than that of couples using other methods. Usually, spermicides are combined with contraceptive barrier methods such as diaphragms, condoms, cervical caps, and sponges. Combined methods are believed to result in lower pregnancy rates than either method alone.

The cervical cap is a form of barrier contraception. A cervical cap fits over the cervix and blocks sperm from entering the uterus through the external orifice of the uterus, called the os.
A pessary is a prosthetic device inserted into the vagina for structural and pharmaceutical purposes. It is most commonly used to treat stress urinary incontinence to stop urinary leakage and to treat pelvic organ prolapse to maintain the location of organs in the pelvic region. It can also be used to administer medications locally in the vagina or as a method of contraception.

The female reproductive system is made up of the internal and external sex organs that function in the reproduction of new offspring. In humans, the female reproductive system is immature at birth and develops to maturity at puberty to be able to produce gametes, and to carry a fetus to full term. The internal sex organs are the vagina, uterus, fallopian tubes, and ovaries. The female reproductive tract includes the vagina, uterus, and fallopian tubes and is prone to infections. The vagina allows for sexual intercourse and childbirth, and is connected to the uterus at the cervix. The uterus or womb accommodates the embryo which develops into the fetus. The uterus also produces secretions which help the transit of sperm to the fallopian tubes, where sperm fertilize ova produced by the ovaries. The external sex organs are also known as the genitals and these are the organs of the vulva including the labia, clitoris, and vaginal opening.

Vaginal rings are polymeric drug delivery devices designed to provide controlled release of drugs for intravaginal administration over extended periods of time. The ring is inserted into the vagina and provides contraception protection. Vaginal rings come in one size that fits most women.

A contraceptive vaginal ring is a type of hormonal insert that is placed in the vagina for the purpose of birth control. The rings themselves utilize a plastic polymer matrix that is inlaid or embedded with contraceptive drug. This drug, often one or two hormones, is absorbed directly through the bloodstream through the cells that line the vaginal wall. Some vaginal rings contain both an estrogen and a progestin, which are available in Europe and the United States. Other vaginal rings contain just progesterone. The progesterone-only ring is only available in Latin America, exclusively for postpartum breastfeeding parents.

There are many methods of birth control that vary in requirements, side effects, and effectiveness. As the technology, education, and awareness about contraception has evolved, new contraception methods have been theorized and put in application. Although no method of birth control is ideal for every user, some methods remain more effective, affordable or intrusive than others. Outlined here are the different types of barrier methods, hormonal methods, various methods including spermicides, emergency contraceptives, and surgical methods and a comparison between them.

An internal condom is a barrier device that is used during sexual intercourse as a barrier contraceptive to reduce the probability of pregnancy or a sexually transmitted infection (STI). Meant as an alternative to the condom, it was invented by Danish MD Lasse Hessel and designed to be worn internally by the woman during vaginal sex to prevent exposure to semen or other body fluids. His invention was launched in Europe in 1990 and approved by the FDA for sale in the US in 1993. Its protection against STIs is inferior to that of male condoms. Internal condoms can be used by the receptive partner during anal sex.

Condom effectiveness is how effective condoms are at preventing STDs and pregnancy. Correctly using male condoms and other barriers like female condoms and dental dams, every time, can reduce the risk of sexually transmitted infections (STIs), including human immunodeficiency virus (HIV) and viral hepatitis. They can also provide protection against other diseases that may be transmitted through sex like Zika and Ebola. Using male or female condoms correctly, every time, can also help prevent pregnancy.

Birth control, also known as contraception, anticonception, and fertility control, is the use of methods or devices to prevent unintended pregnancy. Birth control has been used since ancient times, but effective and safe methods of birth control only became available in the 20th century. Planning, making available, and using human birth control is called family planning. Some cultures limit or discourage access to birth control because they consider it to be morally, religiously, or politically undesirable.
A conception device is a medical device which is used to assist in the achievement of a pregnancy, often, but not always, by means other than sexual intercourse. This article deals exclusively with conception devices for human reproduction.
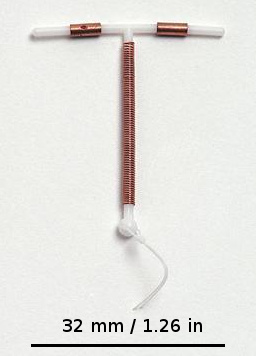
An intrauterine device (IUD), also known as intrauterine contraceptive device or coil, is a small, often T-shaped birth control device that is inserted into the uterus to prevent pregnancy. IUDs are one form of long-acting reversible birth control (LARC). One study found that female family planning providers choose LARC methods more often (41.7%) than the general public (12.1%). Among birth control methods, IUDs, along with other contraceptive implants, result in the greatest satisfaction among users.
There are many types of contraceptive methods available in France. All contraceptives are obtained by medical prescription after a visit to a family planning specialist, a gynecologist or a midwife. An exception to this is emergency contraception, which does not require a prescription and can be obtained directly in a pharmacy.

Cervical drug delivery is a route of carrying drugs into the body through the vagina and cervix. This is a form of localized drug delivery that prevents the drugs from impacting unintended areas of the body, which can lower side effects of toxic drugs such as chemotherapeutics. Cervical drug delivery has specific applications for a variety of female health issues: treatment of cervical cancer, pregnancy prevention, STD prevention, and STD treatment.