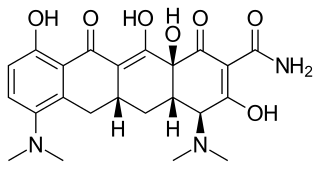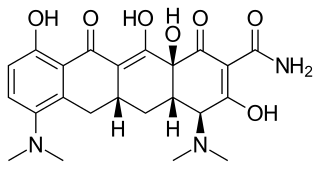
Minocycline, sold under the brand name Minocin among others, is a tetracycline antibiotic medication used to treat a number of bacterial infections such as some occurring in certain forms of pneumonia. It is generally less preferred than the tetracycline doxycycline. Minocycline is also used for the treatment of acne and rheumatoid arthritis. It is taken by mouth or applied to the skin.

Antinuclear antibodies are autoantibodies that bind to contents of the cell nucleus. In normal individuals, the immune system produces antibodies to foreign proteins (antigens) but not to human proteins (autoantigens). In some cases, antibodies to human antigens are produced.

Leukopenia is a decrease in the number of leukocytes (WBC). Found in the blood, they are the white blood cells, and are the body's primary defense against an infection. Thus the condition of leukopenia places individuals at increased risk of infection.

Procainamide (PCA) is a medication of the antiarrhythmic class used for the treatment of cardiac arrhythmias. It is a sodium channel blocker of cardiomyocytes; thus it is classified by the Vaughan Williams classification system as class Ia. In addition to blocking the INa current, it inhibits the IKr rectifier K+ current. Procainamide is also known to induce a voltage-dependent open channel block on the batrachotoxin (BTX)-activated sodium channels in cardiomyocytes.
Warm antibody autoimmune hemolytic anemia (WAIHA) is the most common form of autoimmune haemolytic anemia. About half of the cases are of unknown cause, with the other half attributable to a predisposing condition or medications being taken. Contrary to cold autoimmune hemolytic anemia which happens in cold temperature (28–31 °C), WAIHA happens at body temperature.

Belimumab, sold under the brand name Benlysta, is a human monoclonal antibody that inhibits B-cell activating factor (BAFF), also known as B-lymphocyte stimulator (BLyS). It is approved in the United States and Canada, and the European Union to treat systemic lupus erythematosus and lupus nephritis.

Discoid lupus erythematosus is the most common type of chronic cutaneous lupus (CCLE), an autoimmune skin condition on the lupus erythematosus spectrum of illnesses. It presents with red, painful, inflamed and coin-shaped patches of skin with a scaly and crusty appearance, most often on the scalp, cheeks, and ears. Hair loss may occur if the lesions are on the scalp. The lesions can then develop severe scarring, and the centre areas may appear lighter in color with a rim darker than the normal skin. These lesions can last for years without treatment.
Cerebritis is the inflammation of the cerebrum, which performs a number of important functions, such as memory and speech. It is also defined as a purulent nonencapsulated parenchymal infection of the brain which is characterized by nonspecific features on CT scans and cannot reliably be distinguished from neoplasms.
Drug rash with eosinophilia and systemic symptoms or drug reaction with eosinophilia and systemic symptoms (DRESS), also termed drug-induced hypersensitivity syndrome (DIHS), is a rare reaction to certain medications. It involves primarily a widespread skin rash, fever, swollen lymph nodes, and characteristic blood abnormalities such as an abnormally high level of eosinophils, low number of platelets, and increased number of atypical white blood cells (lymphocytes). However, DRESS is often complicated by potentially life-threatening inflammation of internal organs and the syndrome has about a 10% mortality rate. Treatment consists of stopping the offending medication and providing supportive care. Systemic corticosteroids are commonly used as well but no controlled clinical trials have assessed the efficacy of this treatment.

Lupus erythematosus is a collection of autoimmune diseases in which the human immune system becomes hyperactive and attacks healthy tissues. Symptoms of these diseases can affect many different body systems, including joints, skin, kidneys, blood cells, heart, and lungs. The most common and most severe form is systemic lupus erythematosus.
Sodium channel blockers are drugs which impair the conduction of sodium ions (Na+) through sodium channels.

Anti-double stranded DNA (Anti-dsDNA) antibodies are a group of anti-nuclear antibodies (ANA) the target antigen of which is double stranded DNA. Blood tests such as enzyme-linked immunosorbent assay (ELISA) and immunofluorescence are routinely performed to detect anti-dsDNA antibodies in diagnostic laboratories. They are highly diagnostic of systemic lupus erythematosus (SLE) and are implicated in the pathogenesis of lupus nephritis.
Subacute cutaneous lupus erythematosus is a clinically distinct subset of cases of lupus erythematosus that is most often present in white women aged 15 to 40, consisting of skin lesions that are scaly and evolve as poly-cyclic annular lesions or plaques similar to those of plaque psoriasis.

Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face. Often there are periods of illness, called flares, and periods of remission during which there are few symptoms.
One of the most prevalent forms of adverse drug reactions is cutaneous reactions, with drug-induced urticaria ranking as the second most common type, preceded by drug-induced exanthems. Urticaria, commonly known as hives, manifests as weals, itching, burning, redness, swelling, and angioedema—a rapid swelling of lower skin layers, often more painful than pruritic. These symptoms may occur concurrently, successively, or independently. Typically, when a drug triggers urticaria, symptoms manifest within 24 hours of ingestion, aiding in the identification of the causative agent. Urticaria symptoms usually subside within 1–24 hours, while angioedema may take up to 72 hours to resolve completely.
Drug-Induced Aseptic Meningitis (DIAM) is a type of aseptic meningitis related to the use of medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or biologic drugs such as intravenous immunoglobulin (IVIG). Additionally, this condition generally shows clinical improvement after cessation of the medication, as well as a tendency to relapse with resumption of the medication.
Anti-histone antibodies are autoantibodies that are a subset of the anti-nuclear antibody family, which specifically target histone protein subunits or histone complexes. They were first reported by Henry Kunkel, H.R. Holman, and H.R.G. Dreicher in their studies of cellular causes of lupus erythematosus in 1959–60. Today, anti-histone antibodies are still used as a marker for systemic lupus erythematosus, but are also implicated in other autoimmune diseases like Sjögren syndrome, dermatomyositis, or rheumatoid arthritis. Anti-histone antibodies can be used as a marker for drug-induced lupus.

Anti-SSA autoantibodies are a type of anti-nuclear autoantibodies that are associated with many autoimmune diseases, such as systemic lupus erythematosus (SLE), SS/SLE overlap syndrome, subacute cutaneous lupus erythematosus (SCLE), neonatal lupus and primary biliary cirrhosis. They are often present in Sjögren's syndrome (SS). Additionally, Anti-Ro/SSA can be found in other autoimmune diseases such as systemic sclerosis (SSc), polymyositis/dermatomyositis (PM/DM), rheumatoid arthritis (RA), and mixed connective tissue disease (MCTD), and are also associated with heart arrhythmia.
Dextromethorphan/quinidine, sold under the brand name Nuedexta, is a fixed-dose combination medication for the treatment of pseudobulbar affect (PBA). It contains dextromethorphan (DXM) and the class I antiarrhythmic agent quinidine.
QT prolongation is a measure of delayed ventricular repolarisation, which means the heart muscle takes longer than normal to recharge between beats. It is an electrical disturbance which can be seen on an electrocardiogram (ECG). Excessive QT prolongation can trigger tachycardias such as torsades de pointes (TdP). QT prolongation is an established side effect of antiarrhythmics, but can also be caused by a wide range of non-cardiac medicines, including antibiotics, antidepressants, antihistamines, opioids, and complementary medicines. On an ECG, the QT interval represents the summation of action potentials in cardiac muscle cells, which can be caused by an increase in inward current through sodium or calcium channels, or a decrease in outward current through potassium channels. By binding to and inhibiting the “rapid” delayed rectifier potassium current protein, certain drugs are able to decrease the outward flow of potassium ions and extend the length of phase 3 myocardial repolarization, resulting in QT prolongation.