A ventricle is one of two large chambers toward the bottom of the heart that collect and expel blood towards the peripheral beds within the body and lungs. The blood pumped by a ventricle is supplied by an atrium, an adjacent chamber in the upper heart that is smaller than a ventricle. Interventricular means between the ventricles, while intraventricular means within one ventricle.

Echocardiography, also known as cardiac ultrasound, is the use of ultrasound to examine the heart. It is a type of medical imaging, using standard ultrasound or Doppler ultrasound. The visual image formed using this technique is called an echocardiogram, a cardiac echo, or simply an echo.

Myocarditis, also known as inflammatory cardiomyopathy, is an acquired cardiomyopathy due to inflammation of the heart muscle. Symptoms can include shortness of breath, chest pain, decreased ability to exercise, and an irregular heartbeat. The duration of problems can vary from hours to months. Complications may include heart failure due to dilated cardiomyopathy or cardiac arrest.
Kussmaul's sign is a paradoxical rise in jugular venous pressure (JVP) on inspiration, or a failure in the appropriate fall of the JVP with inspiration. It can be seen in some forms of heart disease and is usually indicative of limited right ventricular filling due to right heart dysfunction.
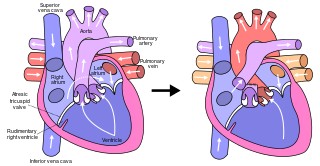
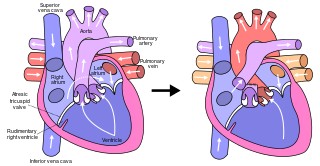
The Fontan procedure or Fontan–Kreutzer procedure is a palliative surgical procedure used in children with univentricular hearts. It involves diverting the venous blood from the inferior vena cava (IVC) and superior vena cava (SVC) to the pulmonary arteries. The procedure varies for differing congenital heart pathologies. For example in tricuspid atresia, the procedure can be done where the blood does not pass through the morphologic right ventricle; i.e., the systemic and pulmonary circulations are placed in series with the functional single ventricle. Whereas in hypoplastic left heart syndrome, the heart is more reliant on the more functional right ventricle to provide blood flow to the systemic circulation. The procedure was initially performed in 1968 by Francis Fontan and Eugene Baudet from Bordeaux, France, published in 1971, simultaneously described in 1971 by Guillermo Kreutzer from Buenos Aires, Argentina, and finally published in 1973.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.

The jugular veins are veins that take deoxygenated blood from the head back to the heart via the superior vena cava. The internal jugular vein descends next to the internal carotid artery and continues posteriorly to the sternocleidomastoid muscle.

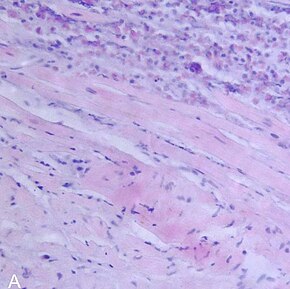
Cardiac amyloidosis is a subcategory of amyloidosis where there is depositing of the protein amyloid in the cardiac muscle and surrounding tissues. Amyloid, a misfolded and insoluble protein, can become a deposit in the heart's atria, valves, or ventricles. These deposits can cause thickening of different sections of the heart, leading to decreased cardiac function. The overall decrease in cardiac function leads to a plethora of symptoms. This multisystem disease was often misdiagnosed, with diagnosis previously occurring after death during autopsy. However, recent advancements of technologies have increased the diagnosis of the disease. Cardiac amyloidosis has multiple sub-types including light chain, familial, and senile. One of the most studied types is light chain cardiac amyloidosis. Prognosis depends on the extent of the deposits in the body and the type of amyloidosis. New treatment methods are actively being researched in regards to the treatment of heart failure and specific cardiac amyloidosis problems.
The following outline is provided as an overview of and topical guide to cardiology, the branch of medicine dealing with disorders of the human heart. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease and electrophysiology. Physicians who specialize in cardiology are called cardiologists.
A bioptome is a small pincer-shaped cutting/grasping instrument used in medicine for taking endomyocardial biopsy specimens of the heart muscle following heart transplantation in rejection monitoring and for diagnosing some diseases of the heart.
Cardiothoracic anesthesiology is a subspeciality of the medical practice of anesthesiology, devoted to the preoperative, intraoperative, and postoperative care of adult and pediatric patients undergoing cardiothoracic surgery and related invasive procedures.
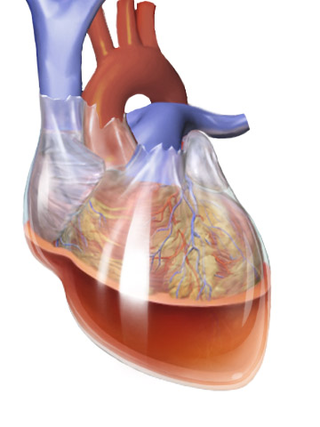
Obstructive shock is one of the four types of shock, caused by a physical obstruction in the flow of blood. Obstruction can occur at the level of the great vessels or the heart itself. Causes include pulmonary embolism, cardiac tamponade, and tension pneumothorax. These are all life-threatening. Symptoms may include shortness of breath, weakness, or altered mental status. Low blood pressure and tachycardia are often seen in shock. Other symptoms depend on the underlying cause.
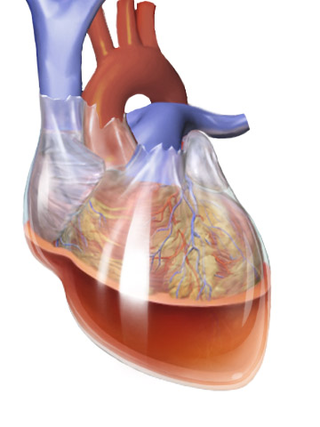
Hemopericardium refers to blood in the pericardial sac of the heart. It is clinically similar to a pericardial effusion, and, depending on the volume and rapidity with which it develops, may cause cardiac tamponade.

A hybrid cardiac surgical procedure in a narrow sense is defined as a procedure that combines a conventional, more invasive surgical part with an interventional part, using some sort of catheter-based procedure guided by fluoroscopy imaging in a hybrid operating room (OR) without interruption. The hybrid technique has a reduced risk of surgical complications and has shown decreased recovery time. It can be used to treat numerous heart diseases and conditions and with the increasing complexity of each case, the hybrid surgical technique is becoming more common.
Sharon Ann Hunt is a cardiology professor and Director of the Post Heart Transplant Programme in Palo Alto, California and is affiliated with Stanford University Medical Center, professionally known for her work in the care of patients after heart transplantation.
Philip Caves (1940–1978) was an Irish cardiothoracic surgeon. In 1972, while at Stanford University, he pioneered the use of the bioptome and transvenous endomyocardial biopsy in the early diagnosis of heart transplant rejection. It was considered the most significant advance in antirejection therapy of the time. Awarded the British American Research Fellowship in 1971, Caves worked with pioneering cardiothoracic surgeon Norman Shumway at Stanford and became staff surgeon leading the transplant programme by 1973. A year later he went to Edinburgh as a senior lecturer in cardiac surgery, where he became particularly interested in pediatric cardiac surgery.

Margaret E. Billingham was a pathologist at Stanford University Medical Center, who made significant achievements in the early recognition and grading of transplant rejection following cardiac transplantation, known as 'Billingham's Criteria'. She also described chronic rejection and techniques in heart endomyocardial biopsy.

Cardiac allograft vasculopathy (CAV) is a progressive type of coronary artery disease in people who have had a heart transplant. As the donor heart has lost its nerve supply there is typically no chest pain, and CAV is usually detected on routine testing. It may present with symptoms such as tiredness and breathlessness.
Percutaneous pulmonary valve implantation (PPVI), also known as transcatheter pulmonary valve replacement (TPVR), is the replacement of the pulmonary valve via catheterization through a vein. It is a significantly less invasive procedure in comparison to open heart surgery and is commonly used to treat conditions such as pulmonary atresia.
Intracardiac echocardiography (ICE) is a specialized form of echocardiography that utilizes an ultrasound-tipped catheter to perform imaging of the heart from within the heart. Unlike transthoracic echocardiography (TTE), ICE is not limited by body habitus. An ICE catheter is inserted into the body, typically, through the femoral vein and advanced into the heart.