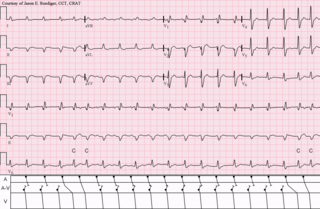
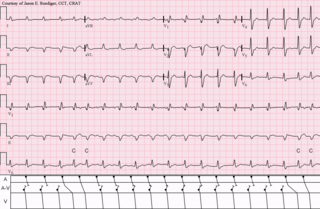
Electrocardiography is the process of producing an electrocardiogram, a recording of the heart's electrical activity through repeated cardiac cycles. It is an electrogram of the heart which is a graph of voltage versus time of the electrical activity of the heart using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including cardiac rhythm disturbances, inadequate coronary artery blood flow, and electrolyte disturbances.

Brugada syndrome (BrS) is a genetic disorder in which the electrical activity of the heart is abnormal due to channelopathy. It increases the risk of abnormal heart rhythms and sudden cardiac death. Those affected may have episodes of syncope. The abnormal heart rhythms seen in those with Brugada syndrome often occur at rest. They may be triggered by a fever.

A premature ventricular contraction (PVC) is a common event where the heartbeat is initiated by Purkinje fibers in the ventricles rather than by the sinoatrial node. PVCs may cause no symptoms or may be perceived as a "skipped beat" or felt as palpitations in the chest. PVCs do not usually pose any danger.

Wolff–Parkinson–White syndrome (WPWS) is a disorder due to a specific type of problem with the electrical system of the heart involving an accessory pathway able to conduct electrical current between the atria and the ventricles, thus bypassing the atrioventricular node. About 60% of people with the electrical problem developed symptoms, which may include an abnormally fast heartbeat, palpitations, shortness of breath, lightheadedness, or syncope. Rarely, cardiac arrest may occur. The most common type of irregular heartbeat that occurs is known as paroxysmal supraventricular tachycardia.

Sinus node dysfunction (SND), also known as sick sinus syndrome (SSS), is a group of abnormal heart rhythms (arrhythmias) usually caused by a malfunction of the sinus node, the heart's primary pacemaker. Tachycardia-bradycardia syndrome is a variant of sick sinus syndrome in which the arrhythmia alternates between fast and slow heart rates.

Palpitations are perceived abnormalities of the heartbeat characterized by awareness of cardiac muscle contractions in the chest, which is further characterized by the hard, fast and/or irregular beatings of the heart.

In medicine, a Holter monitor is a type of ambulatory electrocardiography device, a portable device for cardiac monitoring for at least 24 hours.

Atrial flutter (AFL) is a common abnormal heart rhythm that starts in the atrial chambers of the heart. When it first occurs, it is usually associated with a fast heart rate and is classified as a type of supraventricular tachycardia. Atrial flutter is characterized by a sudden-onset (usually) regular abnormal heart rhythm on an electrocardiogram (ECG) in which the heart rate is fast. Symptoms may include a feeling of the heart beating too fast, too hard, or skipping beats, chest discomfort, difficulty breathing, a feeling as if one's stomach has dropped, a feeling of being light-headed, or loss of consciousness.

Short QT syndrome (SQT) is a very rare genetic disease of the electrical system of the heart, and is associated with an increased risk of abnormal heart rhythms and sudden cardiac death. The syndrome gets its name from a characteristic feature seen on an electrocardiogram (ECG) – a shortening of the QT interval. It is caused by mutations in genes encoding ion channels that shorten the cardiac action potential, and appears to be inherited in an autosomal dominant pattern. The condition is diagnosed using a 12-lead ECG. Short QT syndrome can be treated using an implantable cardioverter-defibrillator or medications including quinidine. Short QT syndrome was first described in 2000, and the first genetic mutation associated with the condition was identified in 2004.

Ventricular tachycardia is a fast heart rate arising from the lower chambers of the heart. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple episodes over a short period of time are referred to as an electrical storm. Short periods may occur without symptoms, or present with lightheadedness, palpitations, or chest pain. Ventricular tachycardia may result in ventricular fibrillation (VF) and turn into cardiac arrest. This conversion of the VT into VF is called the degeneration of the VT. It is found initially in about 7% of people in cardiac arrest.

AV-nodal reentrant tachycardia (AVNRT) is a type of abnormal fast heart rhythm. It is a type of supraventricular tachycardia (SVT), meaning that it originates from a location within the heart above the bundle of His. AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia. It is more common in women than men. The main symptom is palpitations. Treatment may be with specific physical maneuvers, medications, or, rarely, synchronized cardioversion. Frequent attacks may require radiofrequency ablation, in which the abnormally conducting tissue in the heart is destroyed.

Catheter ablation is a procedure that uses radio-frequency energy or other sources to terminate or modify a faulty electrical pathway from sections of the heart of those who are prone to developing cardiac arrhythmias such as atrial fibrillation, atrial flutter and Wolff-Parkinson-White syndrome. If not controlled, such arrhythmias increase the risk of ventricular fibrillation and sudden cardiac arrest. The ablation procedure can be classified by energy source: radiofrequency ablation and cryoablation.

Holiday heart syndrome, also known as alcohol-induced atrial arrhythmias, is a syndrome defined by an irregular heartbeat associated with high levels of ethanol consumption. Holiday heart syndrome was discovered in 1978 when Philip Ettinger discovered the connection between arrythmia and alcohol consumption. It received its common name as it is associated with the binge drinking common during the holidays. It is unclear how common this syndrome is. 5-10% of cases of atrial fibrillation may be related to this condition, but it could be as high 63%.
Premature atrial contraction (PAC), also known as atrial premature complexes (APC) or atrial premature beats (APB), are a common cardiac dysrhythmia characterized by premature heartbeats originating in the atria. While the sinoatrial node typically regulates the heartbeat during normal sinus rhythm, PACs occur when another region of the atria depolarizes before the sinoatrial node and thus triggers a premature heartbeat, in contrast to escape beats, in which the normal sinoatrial node fails, leaving a non-nodal pacemaker to initiate a late beat.
Tachycardia-induced cardiomyopathy (TIC) is a disease where prolonged tachycardia or arrhythmia causes an impairment of the myocardium, which can result in heart failure. People with TIC may have symptoms associated with heart failure and/or symptoms related to the tachycardia or arrhythmia. Though atrial fibrillation is the most common cause of TIC, several tachycardias and arrhythmias have been associated with the disease.
Clinical cardiac electrophysiology, is a branch of the medical specialty of cardiology concerned with the study and treatment of rhythm disorders of the heart. Cardiologists with expertise in this area are usually referred to as electrophysiologists. Electrophysiologists are trained in the mechanism, function, and performance of the electrical activities of the heart. Electrophysiologists work closely with other cardiologists and cardiac surgeons to assist or guide therapy for heart rhythm disturbances (arrhythmias). They are trained to perform interventional and surgical procedures to treat cardiac arrhythmia.

Syncope, commonly known as fainting, or passing out, is a loss of consciousness and muscle strength characterized by a fast onset, short duration, and spontaneous recovery. It is caused by a decrease in blood flow to the brain, typically from low blood pressure. There are sometimes symptoms before the loss of consciousness such as lightheadedness, sweating, pale skin, blurred vision, nausea, vomiting, or feeling warm. Syncope may also be associated with a short episode of muscle twitching. Psychiatric causes can also be determined when a patient experiences fear, anxiety, or panic; particularly before a stressful event, usually medical in nature. When consciousness and muscle strength are not completely lost, it is called presyncope. It is recommended that presyncope be treated the same as syncope.

Atrial fibrillation is an abnormal heart rhythm (arrhythmia) characterized by rapid and irregular beating of the atrial chambers of the heart. It often begins as short periods of abnormal beating, which become longer or continuous over time. It may also start as other forms of arrhythmia such as atrial flutter that then transform into AF.

Arrhythmias, also known as cardiac arrhythmias, heart arrhythmias, or dysrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia, and a resting heart rate that is too slow – below 60 beats per minute – is called bradycardia. Some types of arrhythmias have no symptoms. Symptoms, when present, may include palpitations or feeling a pause between heartbeats. In more serious cases, there may be lightheadedness, passing out, shortness of breath, chest pain, or decreased level of consciousness. While most cases of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in sudden death.
An automatic tachycardia is a cardiac arrhythmia which involves an area of the heart generating an abnormally fast rhythm, sometimes also called enhanced automaticity. These tachycardias, or fast heart rhythms, differ from reentrant tachycardias in which there is an abnormal electrical pathway which gives rise to the pathology. Most automatic tachycardias are supraventricular tachycardias (SVT). It is important to recognize an automatic tachycardia because the treatment will be different to that for a reentrant tachycardia. The most useful clue will be the presence of 'warm up' and 'cool down'. This means that whereas a reentrant tachycardia will both begin and end abruptly as cardiac conduction uses then ceases to use the accessory pathway, an automatic tachycardia will rise and fall gradually in rate as the automatic focus increases and decreases its automatic rate of electrical discharge.