Creutzfeldt–Jakob disease (CJD), also known as subacute spongiform encephalopathy or neurocognitive disorder due to prion disease, is a fatal degenerative brain disorder. Early symptoms include memory problems, behavioral changes, poor coordination, and visual disturbances. Later symptoms include dementia, involuntary movements, blindness, weakness, and coma. About 70% of people die within a year of diagnosis. The name Creutzfeldt–Jakob disease was introduced by Walther Spielmeyer in 1922, after the German neurologists Hans Gerhard Creutzfeldt and Alfons Maria Jakob.

A prion is a misfolded protein that can induce misfolding of normal variants of the same protein and trigger cellular death. Prions cause prion diseases known as transmissible spongiform encephalopathies (TSEs) that are transmissible, fatal neurodegenerative diseases in humans and animals. The proteins may misfold sporadically, due to genetic mutations, or by exposure to an already misfolded protein. The consequent abnormal three-dimensional structure confers on them the ability to cause misfolding of other proteins.
Advanced Sleep Phase Disorder (ASPD), also known as the advanced sleep-phase type (ASPT) of circadian rhythm sleep disorder, is a condition that is characterized by a recurrent pattern of early evening sleepiness and very early morning awakening. This sleep phase advancement can interfere with daily social and work schedules, and results in shortened sleep duration and excessive daytime sleepiness. The timing of sleep and melatonin levels are regulated by the body's central circadian clock, which is located in the suprachiasmatic nucleus in the hypothalamus.

Transmissible spongiform encephalopathies (TSEs) also known as prion diseases, are a group of progressive, incurable, and fatal conditions that are associated with prions and affect the brain and nervous system of many animals, including humans, cattle, and sheep. According to the most widespread hypothesis, they are transmitted by prions, though some other data suggest an involvement of a Spiroplasma infection. Mental and physical abilities deteriorate and many tiny holes appear in the cortex causing it to appear like a sponge when brain tissue obtained at autopsy is examined under a microscope. The disorders cause impairment of brain function, including memory changes, personality changes and problems with movement that worsen chronically.
Hypermetabolism is defined as an elevated resting energy expenditure (REE) > 110% of predicted REE. Hypermetabolism is accompanied by a variety of internal and external symptoms, most notably extreme weight loss, and can also be a symptom in itself. This state of increased metabolic activity can signal underlying issues, especially hyperthyroidism. Patients with Fatal familial insomnia can also present with hypermetabolism; however, this universally fatal disorder is exceedingly rare, with only a few known cases worldwide. The drastic impact of the hypermetabolic state on patient nutritional requirements is often understated or overlooked as well.

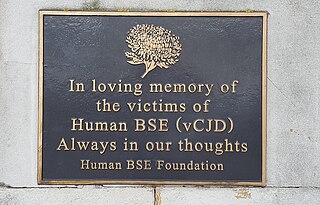
Gerstmann–Sträussler–Scheinker syndrome (GSS) is an extremely rare, always fatal neurodegenerative disease that affects patients from 20 to 60 years in age. It is exclusively heritable, and is found in only a few families all over the world. It is, however, classified with the transmissible spongiform encephalopathies (TSE) due to the causative role played by PRNP, the human prion protein. GSS was first reported by the Austrian physicians Josef Gerstmann, Ernst Sträussler and Ilya Scheinker in 1936.

Major prion protein (PrP) is encoded in the human body by the PRNP gene also known as CD230. Expression of the protein is most predominant in the nervous system but occurs in many other tissues throughout the body.

Fundic gland polyposis is a medical syndrome where the fundus and the body of the stomach develop many fundic gland polyps. The condition has been described both in patients with familial adenomatous polyposis (FAP) and attenuated variants (AFAP), and in patients in whom it occurs sporadically.

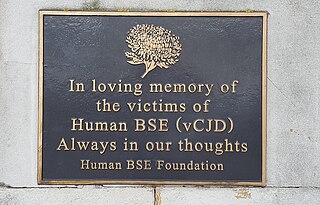
Variant Creutzfeldt–Jakob disease (vCJD), commonly referred to as "mad cow disease" or "human mad cow disease" to distinguish it from its BSE counterpart, is a fatal type of brain disease within the transmissible spongiform encephalopathy family. Initial symptoms include psychiatric problems, behavioral changes, and painful sensations. In the later stages of the illness, patients may exhibit poor coordination, dementia and involuntary movements. The length of time between exposure and the development of symptoms is unclear, but is believed to be years to decades. Average life expectancy following the onset of symptoms is 13 months.

Paroxysmal kinesigenic choreoathetosis (PKC) also called paroxysmal kinesigenic dyskinesia (PKD) is a hyperkinetic movement disorder characterized by attacks of involuntary movements, which are triggered by sudden voluntary movements. The number of attacks can increase during puberty and decrease in a person's 20s to 30s. Involuntary movements can take many forms such as ballism, chorea or dystonia and usually only affect one side of the body or one limb in particular. This rare disorder only affects about 1 in 150,000 people, with PKD accounting for 86.8% of all the types of paroxysmal dyskinesias, and occurs more often in males than females. There are two types of PKD, primary and secondary. Primary PKD can be further broken down into familial and sporadic. Familial PKD, which means the individual has a family history of the disorder, is more common, but sporadic cases are also seen. Secondary PKD can be caused by many other medical conditions such as multiple sclerosis (MS), stroke, pseudohypoparathyroidism, hypocalcemia, hypoglycemia, hyperglycemia, central nervous system trauma, or peripheral nervous system trauma. PKD has also been linked with infantile convulsions and choreoathetosis (ICCA) syndrome, in which patients have afebrile seizures during infancy and then develop paroxysmal choreoathetosis later in life. This phenomenon is actually quite common, with about 42% of individuals with PKD reporting a history of afebrile seizures as a child.
Early-onset Alzheimer's disease (EOAD), also called younger-onset Alzheimer's disease (YOAD), is Alzheimer's disease diagnosed before the age of 65. It is an uncommon form of Alzheimer's, accounting for only 5–10% of all Alzheimer's cases. About 60% have a positive family history of Alzheimer's and 13% of them are inherited in an autosomal dominant manner. Most cases of early-onset Alzheimer's share the same traits as the "late-onset" form and are not caused by known genetic mutations. Little is understood about how it starts.
The National Prion Clinic (UK) is part of the University College London Hospitals NHS Foundation Trust. Its aim is to diagnose and treat patients with any form of human prion disease (Creutzfeldt-Jakob disease, CJD). In addition, the clinic facilitates research in diagnostics and therapeutics, organises clinical trials, and counsels those with an increased genetic risk of the disease.

Variably protease-sensitive prionopathy (VPSPr) is a sporadic prion protein disease first described in an abstract for a conference on prions in 2006, and this study was published in a 2008 report on 11 cases. The study was conducted by Gambetti P., Zou W.Q., and coworkers from the United States National Prion Disease Pathology Surveillance Center. It was first identified as a distinct disease in 2010 by Zou W.Q. and coworkers from the United States National Prion Disease Pathology Surveillance Center.
In biology, a pathogen, in the oldest and broadest sense, is any organism or agent that can produce disease. A pathogen may also be referred to as an infectious agent, or simply a germ.

Kohlschütter–Tönz syndrome (KTS), also called amelo-cerebro-hypohidrotic syndrome, is a rare inherited syndrome characterized by epilepsy, psychomotor delay or regression, intellectual disability, and yellow teeth caused by amelogenesis imperfecta. It is a type A ectodermal dysplasia.
Louis Ptáček is an American neurologist and professor who contributed greatly to the field of genetics and neuroscience. He was also an HHMI investigator from 1997 to 2018. His chief areas of research include the understanding of inherited Mendelian disorders and circadian rhythm genes. Currently, Ptáček is a neurology professor and a director of the Division of Neurogenetics in University of California, San Francisco, School of Medicine. His current investigations primarily focus on extensive clinical studies in families with hereditary disorders, which include identifying and characterizing the genes responsible for neurological variations.

Epstein syndrome is a rare genetic disease characterized by a mutation in the MYH9 gene in nonmuscle myosin. This disease affects the patient's renal system and can result in kidney failure. Epstein syndrome was first discovered in 1972 when two families had similar symptoms to Alport syndrome. Epstein syndrome and other Alport-like disorders were seen to be caused by mutations in the MYH9 gene, however, Epstein syndrome differs as it was more specifically linked to a mutation on the R702 codon on the MYH9 gene. Diseases with mutations on the MYH9 gene also include May–Hegglin anomaly, Sebastian syndrome and Fechtner syndrome.
The United Kingdom was afflicted with an outbreak of Bovine spongiform encephalopathy, and its human equivalent variant Creutzfeldt–Jakob disease (vCJD), in the 1980s and 1990s. Over four million head of cattle were slaughtered in an effort to contain the outbreak, and 178 people died after contracting vCJD through eating infected beef. A political and public health crisis resulted, and British beef was banned from export to numerous countries around the world, with some bans remaining in place until as late as 2019.
Familial sleep traits are heritable variations in sleep patterns, resulting in abnormal sleep-wake times and/or abnormal sleep length.

Familial natural short sleep is a rare, genetic, typically inherited trait where an individual sleeps for fewer hours than average without suffering from daytime sleepiness or other consequences of sleep deprivation. This process is entirely natural in this kind of individual, and it is caused by certain genetic mutations. A person with this trait is known as a "natural short sleeper".

![Hypnogram comparing the sleep pattern of a healthy control with five FFI patients, who display decreased sleep efficiency and disrupted sleep cycles. [W: wake; R: REM; N1-3: NREM sleep stages]. FFI Diagrams.svg](http://upload.wikimedia.org/wikipedia/commons/thumb/0/0c/FFI_Diagrams.svg/220px-FFI_Diagrams.svg.png)